Research - (2025) Volume 20, Issue 1
*Correspondence: Dr. Haider Osman Ibn Idris Elmisbah, Department of Surgery, Northern Border University Arar, Saudi Arabia, 73241, Saudi Arabia, Email:
2Department of Medicine, Northern Border University Arar, Saudi Arabia, 73241, Saudi Arabia
3Intern Medical doctor, Northern Border University Saudi Arabia, Saudi Arabia
Received: 20-Jan-2025 Published: 12-Feb-2025
Abstract
Objectives: To assess the effectiveness and safety of Aquablation therapy for the management of benign prostatic hyperplasia (BPH).
Methods: A comprehensive examination of four databases revealed 366 pertinent publications. Following the elimination of duplicates via the Rayyan QCRI and the assessment of relevance, 49 full-text publications were examined, of which five satisfied the eligibility criteria for evidence synthesis.
Results: Five studies on 1004 patients with BPH found that aquablation therapy was effective and comparable to or better than transurethral resection of the prostate (TURP) and holmium laser enucleation of the prostate (HoLEP). It alleviates urinary symptoms, maintains sexual function, and reduces retrograde ejaculation. Early complications such as hemorrhage and urinary retention are rare. Aquablation is a sustainable and less intrusive solution.
Conclusion: Aquablation therapy is a promising advancement in BPH treatment, as it provides lasting symptomatic relief and preserves sexual function. It effectively treats large prostate tumors with few side effects, making it a strong alternative to TURP and HoLEP. Although early complications can occur, their longterm benefits and minimally invasive nature have increased their appeal. Ongoing research and validation are expected to confirm the Aquablation’s role of ablation in BPH management.
Keywords
Aquablation therapy; Benign prostatic hyperplasia; BPH treatment; Systematic review
Introduction
Benign prostatic hyperplasia (BPH) is a nonmalignant enlargement of the prostate gland induced by androgenic stimulation from dihydrotestosterone, a testosterone by-product generated by the enzyme 5-alpha reductase [1]. The primary risk factors for BPH are age, presence of functional testicles due to hormonal influences, familial history of the condition, and obesity [2]. Fifty percent of men aged 60 years and 90 percent of men aged 85 years exhibit microscopic benign prostatic hyperplasia (BPH). Among individuals with this histological outcome, only 50 percent will exhibit macroscopic gland enlargement, and approximately half of them manifest symptoms [3]. Prostate enlargement is merely one factor linked to the manifestation of symptoms; thus, the most suitable term for this phenomenon is "lower urinary tract symptom " (LUTS). Between 10% and 30% of men aged 60 to 70 and 30% of men aged 80 experience lower urinary tract symptoms (LUTS) [4].
Research indicates that aquablation is as successful as TURP, in both subjective and objective assessments. However, post treatment hemostasis remains an issue. The European Association of Urology (EAU) guidelines include aquablation as a surgical alternative to prostate ablation [5].
BPH is one of the most common problems among aging males, mostly presenting with symptoms of the lower urinary tract that have great effects on quality of life. Conventional surgical procedures, including transurethral resection of the prostate and holmium laser enucleation, result in sexual dysfunction, incontinence, and prolonged recovery times as major drawbacks. Aquablation therapy is a novel, minimally invasive technique that uses highvelocity water jets under robotic guidance and is emerging as a promising alternative offering precise tissue removal while preserving the surrounding structures. As clinical adoption continues to grow, understanding the efficacy and safety profile of Aquablation is critical for guiding treatment decisions and optimizing patient outcomes.
This systematic review aimed to determine the efficacy and safety of Aquablation in BPH treatment. This review summarizes the data from clinical studies that have assessed changes in urinary symptoms, uroflow parameters, and prostate volume reduction. Complication rates, bleeding, urinary retention, and sexual dysfunction will be analyzed using Aquablation and compared with conventional therapies to define its role in the treatment of BPH.
Methods
Search strategy
This systematic review complied with the PRISMA and GATHER guidelines. A thorough investigation was conducted to identify relevant studies on the effectiveness and safety of Aquablation therapy for benign prostatic hyperplasia (BPH). The reviewers searched four electronic databases, SCOPUS, Web of Science, Cochrane Library, and PubMed. We included controlled trials published in the last five years (2019-2024). We removed duplicates and uploaded all titles and abstracts identified by electronic searches in Rayyan. Subsequently, all study materials that met the inclusion criteria based on the abstract or title were collected for thorough assessment of the full text. Two reviewers independently evaluated the suitability of the selected studies and discussed discrepancies.
Study population-selection
The population, intervention, comparator, and outcome (PICO) components were defined as the inclusion criteria for our review: (i) population: Males diagnosed with benign prostatic hyperplasia (BPH) presenting with lower urinary tract symptoms (LUTS); (ii) intervention: aquablation therapy; (iii) Comparison: Conventional therapies including TURP or HoLEP; and (iv) Outcome: Effectiveness and adverse effects.
Data extraction
Data from studies that satisfied the inclusion criteria were acquired by two impartial reviewers in a standardized manner. The following information was obtained and documented: (i) lead author; (ii) publication year; (iii) research technique; (iv) study nation; (v) sample size; (vi) age range; (vii) sex; (viii) follow-up period (in years); (ix) comparator group; (x) prostate volume; (xi) complications; and (xii) primary outcomes.
Quality review
Owing to the prevalence of bias from omitted variables in this domain, we employed the ROBINS-I methodology to evaluate the potential for bias as it facilitates a comprehensive analysis of confounding factors. The ROBINS-I tool is intended for cohort studies that monitor people subjected to varying staffing levels over time and seeks to evaluate non-randomized research. The risk of bias for each paper was individually assessed by two reviewers, with any discrepancies addressed through group discussion [6].
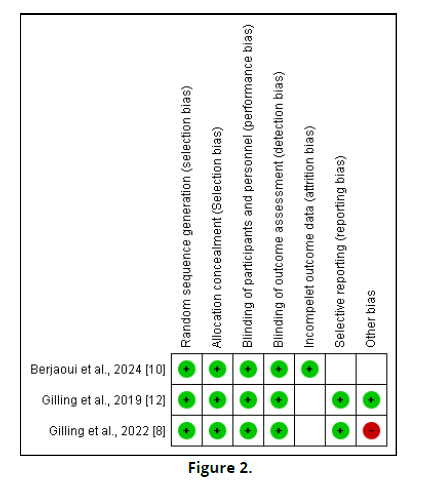
The Cochrane Risk of Bias Instrument [7] was used to rigorously evaluate the selected randomized controlled trials. This instrument assesses the risk of bias across seven domains: random sequence generation, allocation concealment, participant and personnel blinding, outcome assessment blinding, insufficient outcome data, selective reporting, and other sources of bias. The risk of bias in each category was categorized as low, unclear, or high.
Results
The search yielded 366 publications (Figure 1). After eliminating duplicates (n = 180), 200 trials were assessed since their titles and abstracts. Of these, 149 did not meet the qualifying criteria, resulting in 51 full-text publications that were available for a thorough review. Five individuals met the eligibility criteria for the evidence synthesis (Figure 2, 3).
Sociodemographic and clinical outcomes
We included five trials, including a total of 1004 patients with BPH, 532 patients receiving aquablation therapy, and 472 patients undergoing other surgical interventions. Three studies were randomized controlled trials [8, 10, 12], one was a non-randomized controlled trial [9], and one was a case-control study [11]. Two studies were conducted in the USA [8, 12], two in Germany [9, 11], and one in Canada [10]. The follow-up duration in this study ranged from one year [9, 12] to five years [8, 10].
Main Clinical outcomes
Aquablation therapy consistently demonstrates positive clinical outcomes, including sustained symptom relief, improved urinary flow rates, and a reduced need for secondary interventions [8]. The effectiveness of the therapy appears particularly pronounced in patients with larger prostate volumes (≥50 mL), where it shows superior results compared with traditional treatments [8]. Additionally, Aquablation offers significant benefits in preserving sexual function with lower rates of retrograde ejaculation, making it an attractive option for patients concerned about this side effect [12]. Long-term followup data indicate that improvements in uroflow metrics and quality of life are maintained for several years, reinforcing the role of aquablation as a durable and effective treatment for BPH [10] (Table 1 & 2).
| Study ID | Country | Study design | Sociodemographic | Follow-up (years) | Comparator | Prostatic volume (cc) | Complications | Main outcomes |
|---|---|---|---|---|---|---|---|---|
| Gilling et al., 2022 [8] | USA | RCT | Cases= 116 Controls= 65 Mean age: 66 |
5 | TURP | 54.1 (16.2) | No complications were reported | Aquablation offers better outcomes than TURP by reducing the need for secondary BPH treatment, preventing retrograde ejaculation, and providing sustained symptom and uroflow improvements. It also shows greater safety and effectiveness, especially for larger prostates (≥ 50 mL). |
| Michaelis et al., 2024 [9] | Germany | Non-randomized control trial | Cases= 16 Controls= 24 Mean age: 66.3 |
1 | HoLEP | 66.3 | While only one patient in the HoLEP group experienced CD-grade 3b problems, six patients in the aquablation group did. | At three months, aquablation showed short-term improvements in ejaculation and continence. |
| Berjaoui et al., 2024 [10] | Canada | RCT | Cases= 116 Controls= 101 Mean age: 65.9 |
5 | Water II | 54.1 (16.3) | Any treatment for urethral strictures was not taken into consideration because the surgical retreatment rate was considered as needing surgery for BPH. | Across a range of prostate sizes and shapes, aquablation therapy reliably produces normalized clinical effects. Regardless of prostate size, Aquablation offers favorable clinical results, quick learning curves, and shorter operating times. |
| Golger et al., 2021 [11] | Germany | Case-control | Cases= 167 Controls= 215 Mean age: 65.7 |
NM | HoLEP | 56.2 (24.5) | the risk of blood loss during surgery, postoperative reinterventions, or blood transfusions following Aquablation and selective transurethral hemostasis is the same as that of HoLEP. | Aquablation therapy is as effective as HoLEP |
| Gilling et al., 2019 [12] | USA | RCT | Cases= 117 Controls= 67 Mean age: 66 |
1 | TURP | 54.1 (16.2) | Early complications included bleeding (15.5%) and dysuria (10.3%) being the most prevalent within three months. Urinary retention, infections, and retrograde ejaculation affect a smaller subset (6-9.5%). | For men with prostates between 30 and 80 cc, aquablation for LUTS caused by BPH offers long-lasting (12-month) symptom-reduction effectiveness with a low rate of late side effects. For men who want to preserve their ability to ejaculate, aquablation might be a good substitute. |
| Study ID | Bias due to confounding | Bias in theselection of participants into | Bias in theclassification of interventions | Bias due to deviations from theintended interval | Bias due to missing data | Bias in themeasurement of outcomes | Bias in theselection of reported result | Overall bias |
|---|---|---|---|---|---|---|---|---|
| Michaelis et al., 2024 [9] | Mod | Low | Low | Low | Low | Mod | Low | Low |
| Golger et al., 2021 [11] | Mod | Low | Mod | Low | Low | Mod | Low | Moderate |
Complications
The complication rates associated with Aquablation therapy vary across studies, with some reporting no significant adverse events [8], while others highlight early post-procedural issues, such as bleeding, dysuria, and urinary retention, typically occurring within the first three months [12]. In a few cases, more severe complications such as urethral damage or strictures were observed, although these were infrequent [9]. Comparisons with alternative procedures, such as HoLEP, revealed that while the incidence of complications may differ slightly, the overall risk profile remains comparable [11]. The presence of bleeding and other early complications suggests the need for vigilant postoperative monitoring; however, the absence of major long-term adverse effects indicates a favorable safety profile for Aquablation [8].
Discussion
TURP is a superior surgical option for prostate volumes of 80–100 ml, as alternative methods such as transurethral incision of the prostate (TUIP), transurethral microwave therapy (TUMT), and transurethral needle ablation of the prostate (TUNA) demonstrate limited effectiveness, technical difficulties, and perioperative complications [13, 14]. This occurs despite the potential complications associated with TURP. Direct prostatectomy, which entails a heightened risk of complications, is the preferred endoscopic surgical approach for managing enlarged prostates owing to the increased complication rate associated with TURP and the protracted learning curve required to attain satisfactory outcomes with techniques such as Green Light (GL) and HOLEP [15].
This review found that Aquablation therapy has recently been developed as a strong alternative to traditional surgical management of BPH. It has demonstrated precision in prostate tissue removal with minimal destruction of the surrounding structures, thus achieving positive clinical outcomes in preserving sexual function and minimizing the risk of retrograde ejaculation [12]. This fact proves the effectiveness of the procedure across a range of prostate sizes, although significant benefits in larger glands ≥50 mL are clear where conventional methods such as TURP carry increased risks and longer operative times [8, 10].
Saadat et al. reported that a larger prostate diameter does not influence the functional outcomes of Aquablation. Aquablation consistently provides equivalent benefits, even for prostates of up to 150 ml, and TURP's effectiveness of TURP is limited to a prostate volume of 100 ml, despite both procedures demonstrating similar results in the WATER study. The importance of this is further illustrated by comparing the user-friendliness of the Aqua Beam system with the learning curve associated with HoLEP and GL for enlarged prostates [16]. The surgeon's principal duty when utilizing Aqua Beam technology is to delineate the ablation field via TRUS while the ablation segment of the procedure is executed robotically. Compared to the skills required to proficiently perform efficient GL or HoLEP on an enlarged prostate, TRUS is significantly simpler to acquire and replicate, as it is widely acquainted with most urologists [17].
Nedbal et al. conducted a scoping review, indicating that aquablation is an effective treatment for BPH with the potential to become a standard of care. The procedure is now implemented at certain locations, and extensive dissemination has yet to be achieved. Aquablation, characterized by a favorable safety profile and suitability for all prostate sizes and patient ages, yields positive functional outcomes, including optimal preservation of ejaculatory function and a persistent reduction in LUTS over five years [18].
Our review reported that early complications, such as bleeding and urinary retention, still occurred, although the vast majority of these were self-limiting and at similar rates as HoLEP and TURP [9, 11]. Saadat et al. found that with the preservation of ejaculatory function and a safety profile that appears to outperform other choices for individuals with greater prostate volumes, aquablation appears to be a potential option for the treatment of LUTS arising from BPE in patients with varying prostate sizes [16].
Clinical Implications: Aquablation therapy has significant clinical implications and provides a minimally invasive alternative that effectively reduces urinary symptoms while preserving key aspects of sexual function. This makes it particularly valuable for men experiencing moderate-to-severe lower urinary tract symptoms who wish to avoid sexual side effects that are often associated with more invasive procedures. In addition, the fact that Aquablation is effective in larger prostate glands expands its utility to patients who may require more complex surgical interventions. For clinicians, the smaller learning curve and shorter operative times with Aquablation provide practical advantages that enhance accessibility and, by extension, the range of patient treatment options in both high-volume and community health care settings. Long-term effectiveness translates into wider recognition of therapy, which might establish a cornerstone for further advances in BPH therapy.
Strengths
It reviews the available evidence on Aquablation therapy regarding its effectiveness and safety in the management of BPH compared to traditional treatments. This paper is a comprehensive synthesis because it incorporates several study designs, including, but not limited to, randomized controlled trials and observational studies that provide outcomes from both controlled studies and those that reflect real-world experience. A detailed analysis of the results, including symptomatic relief, preservation of sexual function, and longterm durability, will be instructive for clinicians and researchers. In addition, this review summarizes the efficacy of Aquablation for various prostate sizes and provides practical guidelines for its use in different patient populations. The inclusion of complications and their context in relation to other therapies strengthens the analysis and provides a subtler understanding of the riskbenefit profile of the therapy.
Limitations
Nevertheless, this review has several limitations, such as variability in the included studies regarding patient populations, follow-up duration, and outcome measures. Most data are from only a few randomized controlled trials and observational studies and are not fully representative of the spectrum of Aquablation outcomes. Moreover, most studies have reported a relatively short follow-up time, which restricts any comprehensive assessment of longterm safety and efficacy. The review also faces challenges in directly comparing Aquablation with HoLEP and TURP, because head-to-head studies are limited in number and scope. Potential publication bias and exclusion of unpublished or non-English studies may further limit the generalizability of the findings. Finally, although complications were reported, variability in how they were defined and measured across studies complicated the direct comparisons, potentially affecting the reliability of the conclusions drawn.
Conclusion
Aquablation therapy represents a significant advancement in the surgical treatment of BPH, offering durable symptom relief, preserving sexual function, and demonstrating a favorable safety profile. Its ability to effectively treat larger prostate glands while minimizing sexual side effects is a valuable alternative to traditional methods, such as TURP and HoLEP. Although early complications remain to be considered, the long-term benefits of Aquablation, together with its minimally invasive approach, are becoming increasingly attractive to both patients and clinicians. Further research and clinical validation are required to expand the understanding of the role of Aquablation.
References
Partin AW, Peters CA, Kavoussi LR, Dmochowski RR, Wein AJ. Campbell Walsh Wein Urology: 4-Volume Set. Elsevier; 2020.
Ng M, Baradhi KM. Benign Prostatic Hyperplasia. In: StatPearls. StatPearls Publishing; 2022.
Gupta NK, Gange SN, McVary KT. New and Emerging Technologies in Treatment of Lower Urinary Tract Symptoms From Benign Prostatic Hyperplasia. Sex Med Rev. 2019 Jul;7(3):491-498.
Parsons JK, Bergstrom J, Silberstein J, Barrett-Connor E. Prevalence and characteristics of lower urinary tract symptoms in men aged > or ¼ 80 years. Urology 2008;72(2):318e21.
Cornu J, Gacci M, Hashim H, et al. EAU guidelines on non-neurogenic male lower urinary tract symptoms (LUTS) incl. benign prostatic obstruction (BPO). Arnhem, The Netherlands: European Association of Urology; 2023. p. 42–3. https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Non-Neurogenic-Male-LUTS-2023.pdf
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. bmj. 2016 Oct 12;355.
Jørgensen L, Paludan-Müller AS, Laursen DR, Savović J, Boutron I, Sterne JA, Higgins JP, Hróbjartsson A. Evaluation of the Cochrane tool for assessing risk of bias in randomized clinical trials: overview of published comments and analysis of user practice in Cochrane and non-Cochrane reviews. Systematic reviews. 2016 Dec;5:1-3.
Gilling PJ, Barber N, Bidair M, Anderson P, Sutton M, Aho T, Kramolowsky E, Thomas A, Kaufman RP, Badlani G. Five-year outcomes for Aquablation therapy compared to TURP: results from a double-blind, randomized trial in men with LUTS due to BPH. Can J Urol. 2022 Feb 1;29(1):10960-8.
Michaelis J, Träger M, Astheimer S, von Büren M, Gabele E, Grabbert M, Halbich J, Kamps M, Klockenbusch J, Noll T, Pohlmann P. Aquablation versus HoLEP in patients with benign prostatic hyperplasia: a comparative prospective non-randomized study. World Journal of Urology. 2024 May 9;42(1):306.
Berjaoui MB, Nguyen DD, Almousa S, Daher K, Barber N, Bidair M, Gilling P, Anderson P, Zorn KC, Badlani G, Humphreys M. WATER versus WATER II 5‐year update: Comparing Aquablation therapy for benign prostatic hyperplasia in 30–80‐cm3 and 80–150‐cm3 prostates. BJUI compass. 2024 Nov;5(11):1023-33.
Gloger S, Schueller L, Paulics L, Bach T, Ubrig B. Aquablation with subsequent selective bipolar cauterization versus holmium laser enucleation of the prostate (HoLEP) with regard to perioperative bleeding. Can J Urol. 2021 Jun 1;28(3):10685-90.
Gilling PJ, Barber N, Bidair M, Anderson P, Sutton M, Aho T, Kramolowsky E, Thomas A, Cowan B, Roehrborn C. Randomized controlled trial of aquablation versus transurethral resection of the prostate in benign prostatic hyperplasia: one-year outcomes. Urology. 2019 Mar 1;125:169-73.
Oelke M, Bachmann A, Descazeaud A, et al. members of the EAU Guidelines Panel. EAU guidelines on management of nonneurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO) E. Retreived from https://uroweb. org/guideline/treatment-of-non-neurogenic-male-luts/. https://doi. org/10.1007/s10126-007-9056-7. Accessed Dec 2024.
Gilling PJ, Barber N, Bidair M, Anderson P, Sutton M, Aho T, Kramolowsky E, Thomas A, Kaufman RP Jr, Badlani G, Plante M, Desai M, Doumanian L, Te AE, Roehrborn CG. Five-year outcomes for Aquablation therapy compared to TURP: results from a double-blind, randomized trial in men with LUTS due to BPH. Can J Urol. 2022 Feb;29(1)..
Rapisarda S, Russo GI, Osman NI, Chapple CR, Morgia G, Tubaro A, Esperto F; EAU-ESRU (European Associations of Urology-European Society of Residents Urologist). The use of laser as a therapeutic modality compared to TURP for small prostate volume ≤40 mL: A collaborative review. Minerva Urol Nefrol. 2019 Dec;71(6):569-575. doi: 10.23736/S0393-2249.19.03350-2. Epub 2019 Apr 5. PMID: 30957474..Saadat H, Elterman DS. Role of aqua ablation in the surgical treatment of LUTS/BPH. Current urological reports. 2019 Aug;20:1-8.
Valdivieso R, Hueber P-A, Meskawi M, Belleville E, Ajib K, Bruyere F, et al. international experience with 532-nm laser photoselective vaporization with GreenLight XPS in men with very large prostates. BJU Int. 2018;122(5):873–8.
Nedbal C, Castellani D, De Stefano V, Giulioni C, Nicoletti R, Pirola G, Teoh JY, Elterman D, Somani BK, Gauhar V. Will Aquablation Be the New Benchmark for Robotic Minimally Invasive Surgical Treatment for Benign Prostatic Hyperplasia?. European Urology Focus. 2023 Dec 29.
Nedbal C, Castellani D, De Stefano V, Giulioni C, Nicoletti R, Pirola G, Teoh JY, Elterman D, Somani BK, Gauhar V. Will Aquablation Be the New Benchmark for Robotic Minimally Invasive Surgical Treatment for Benign Prostatic Hyperplasia?. European Urology Focus. 2023 Dec 29.