Research Article - (2024) Volume 19, Issue 3
*Correspondence: Maha G. Ibrahim, Lecturer, Department of Physical Therapy for Basic Sciences, Faculty of Physical Therapy, Modern Universityfor Technology and Information, Cairo, Egypt, Email:
2Assistant Professor, Department of Physical Therapy for Orthopedic and Orthopedic Surgery, Badr University in Cairo, Egypt
3Lecturer of Physical Therapy for Pediatrics and Surgery, Modern University for Technology and Information University, Cairo, Egypt
4Lecturer of Physical Therapy, Women’s Health Department, Modern University for Technology and Information, Cairo, Egypt
5Lecturer of Physical Therapy at Department of Neurology and its Surgery, Faculty of Physical Therapy, Al Ryada University for Science and Technology, , Egypt
6Lecturer at Basic science Department, Faculty of Physical Therapy, Heliopolis University for Sustainable Development, Cairo, Egypt
Received: 03-Jun-2024 Published: 18-Jun-2024
Abstract
Objectives: To compare the impact of core stability exercises versus Biodex balance training on postural stability and sway among patients suffering from mechanical low back pain.
Methods: The study was conducted in the outpatient clinic of the Faculty of Physical Therapy, Modern University for Technology and Information, between March and June 2023. This randomized, double?blind, pre?post measurement study included forty-eight patients have been participated in this study and divided into three groups, Group A (control group) (n = 18) were given stretching as well as strengthening exercises. Group B (n = 18) were given core stability exercises plus stretching as well as strengthening exercises. Group C (n = 18) were given Biodex balance training (limit of stability, maze, and random control modes training) plus stretching as well as strengthening exercises. The Biodex Balance System were utilized to quantify dynamic balance indices at baseline and six weeks following therapy. Statistical analysis among groups for eye open firm, eye closed firm, eye open foam, and eye closed foam revealed from the Modified clinical test of sensory interaction and balance which were the main outcome indicator.
Results: The Within-Group analysis revealed substantial differences regarding postural stability as well as control of postural sway for groups B and C, both prior to and following the treatment program (p value < 0.05). The between-group analysis revealed statistically substantial variations across all variables following the therapy, with Group C exhibiting further pronounced differences compared to Groups A and B (p < 0.05).
Conclusion: Enhancement in all measures of dynamic balance was shown following core stability training activities and Biodex balance training, with a greater degree of improvement seen after Biodex balance training.
Keywords
Biodex, Core stability exercises, Stretching, and Mechanical low back pain.
Introduction
Mechanical low back pain (MLBP) is a significant musculoskeletal problem which results in clinical, social, along with economic complications. 1 MLBP commonly affecting up to 85%, 90% of population.2, 3 Approximately two-thirds of adults are believed to have or have experienced MLBP at some stage in their lifetime, with up to 50% reporting recurring complaints of MLBP .4
Core stabilization exercises (CSE) Over the years, the usage of MLBP treatments has grown increasingly popular and extensively adopted. These treatments aim to lessen pain severity along with enhance muscular function among individuals suffering from MLBP.5 The core stability muscles can be defined as a muscular structure consisting of the abdominal anteriorly, paraspinals & gluteal muscles posteriorly, with the diaphragm as the superior boundary, and the pelvic floor as the inferior boundary. Inside this enclosure, there exist 29 sets of muscles that aid in the stabilisation of the spine.2
Core stability muscles give corset-like support, resulting in a stable spine. This concept comes from the functional anatomy of the core musculature, which shows that increasing intra-abdominal pressure causes rigidity of the stabilising muscles. The transverse abdominus as well as multifidus muscles are the main causes of intraabdominal pressure. 6 The core is a muscular cylinder, with the abdominals anteriorly, the paraspinal as well as gluteal muscles posteriorly, the diaphragm creating the roof, and the pelvic floor muscles making the floor.7
An effective CSE should take into account both the motor and sensory aspects of the exercise in order to enhance spinal stability to the highest degree.8 CSE have emerged as a favoured fitness trend that has been incorporated into sports medicine and rehabilitation programmes. 2,4. It is controlled by sensory information (vestibular, visual, cutaneous as well as proprioceptive), neuromuscular responses and central processing. 9 CSE can also improve balance performance and pain intensity specially for deep abdominal muscle. Postural control is a crucial element of motor skill and a necessary condition for coordination. 10
CSE is crucial for effectively carrying out daily tasks, improving overall performance, and mitigating the risk of injury. Both the maintenance and recovery of balance are controlled by two mechanisms that make up postural stability.11 Both outcomes are achievable as a result of the synchronized actions of postural muscles, which include the muscles that make up the core.
Stretching exercises showed greater decreases in pain as well as functional disability. A regimen of 12 strengthening exercises has been found to be highly helpful in alleviating pain, enhancing proprioception, balance, as well as how much the Transversus abdominus as well as multifidus muscles have changed in thickness. Additionally, it has been shown to reduce disability and fear of movement among individuals suffering from LBP.13
Biodex Balance System (BBS) indices are considered reliable indicators of postural control among patients suffering from LBP, particularly in more difficult situations, like when standing with eyes closed.14 By using the BBS, the patients can test and train their balance and enhance their neuromuscular control, as it has a platform with adjustable stability settings. Proprioceptive training as well as balancing exercises employing the Biodex stability device have been shown to increase elderly people's standing balance and mobility while decreasing their risk of falling, according to the available literature.15
The study seeks to evaluate the efficacy of training using the Biodex balancing system and core stability exercises postural sway, dynamic postural stability in mechanical low back pain patients to obtain the best treatment results.
Materials And Methods
Study Design
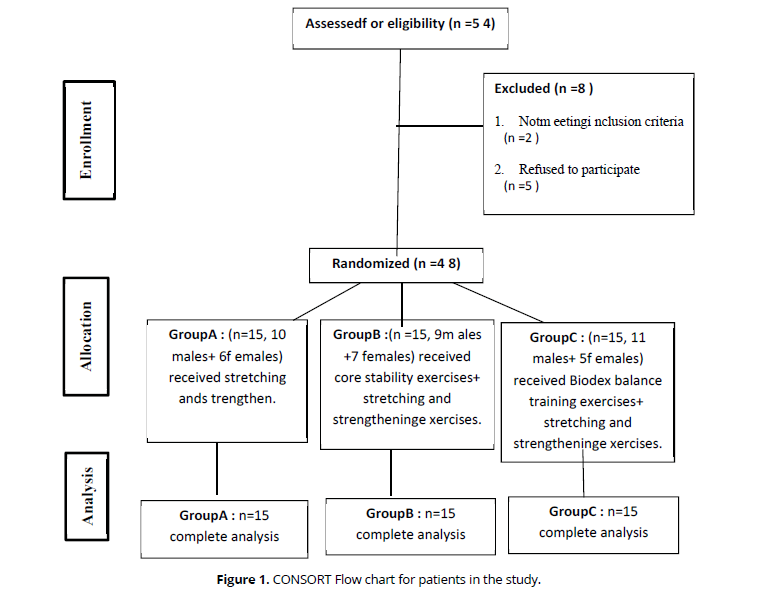
This study, a randomized controlled trial, contrasted the impacts of core stability exercises and Biodex balance training on posture stability, postural sway, and dynamic postural stability in mechanical low back pain patients. It was carried out at the outpatient clinic Faculty of Physical Therapy, Modern University for Technology and Information from March to June 2023. Consolidated Standards of Reporting Trials (CONSORT) reporting standards were used in this study. The G Power statistical programme (version 3.1.9.2) was utilised to determine the required sample size for the study. The calculations were based on F tests, specifically for repeated measurements with both within-between variables. The significance level (α) was set at 0.05, the power (β) at 0.2, and the medium effect size at 0.24. The software determined that a sample size of 48 was adequate for the study. The primary outcome measure was the test results obtained from the mCTSIB. The study has included 48 patients in all (Figure 1).
Patient characteristics
Following the signing of a consent form, 45 patients (18 female and 30 male) were randomly partitioned into three equal groups. The therapist recruited 58 patients who were eligible to participate in the trial and instructed them to select an envelope at random before the experiment began. Out of the 48 sealed envelopes, 16 had letter (A) inside, 16 had letter (B) inside, and 16 had letter (C) inside; the overall number for each group was then calculated.
Group A were given stretching as well as strengthening exercises. Group B were given CSE plus stretching as well as strengthening exercises. Group C were given Biodex balance training (limit of stability, maze, as well as random control modes training) in addition stretching as well as strengthening exercises. The requirements for inclusion were as follows: (1) Patients between the ages of 20 and 40,1 There are no observable consequences of the arthritic alterations that have occurred in the joints of the lumbar spine;16 (2) Participants who had many episodes of MLBP within the six months preceding the research;17 (3) Patients with a BMI >30 kg/m2 have poorer balance and mobility because higher BMI levels.18
The following were the exclusion criteria:(1) Patients suffering from vestibular as well as Neurological disorders; (2) Patients who have recently received steroid injection therapy for a systemic inflammatory disease within the past 6 months;19 (3) Patients with a prior surgical history involving the musculoskeletal parts of the spine;19 (4) Individuals who have experienced recent acute injury to the musculoskeletal structures in the spinal joints within the past three months.20 (5) lumber disc problems or cervical spondylosis.20
Procedure Evaluations The same therapist completed all assessments both before and after the treatment programme was complete. The Biodex Balance SystemTM SD (BBS) (Biodex Medical Systems Inc., New York, USA) is a valid as well as reliable tool for quantifying postural sway along with the dynamic postural stability.21 The Biodex System is a multiaxial apparatus which measures then documents the subject's ability to maintain their posture while experiencing both dynamic and static stress. The structure consists of a circular platform capable of movement in all four directions: ant., post., medial, as well as lateral. The platform's stability can be modified on a scale from level 1, which represents the lowest stability, to level 12, which represents the highest stability.22 In this study, we used the (m‐CTSIB).
Modified Clinical Test of Sensory interaction and Balance (m‐CTSIB):
The test was designed to evaluate the incorporation of visual, somatosensory, as well as vestibular stimuli in order to sustain balance as well as stability of posture.22 Furthermore, this test is highly efficient in detecting patients who have mild to severe balance impairments, as it specifically identifies the damaged system. 23 The test is widely regarded as a valid as well as reliable method for the measurement of postural sway. 24 This test consisted of 4 conditions: (1) Opened eyes, Firm Surface, (2) Closed eyes, Firm Surface, (3) Opened eyes, Foam Surface, as well as (4) Closed eyes, Foam Surface. Beginning from the starting point of the preceding test, each condition was performed twice for a period of thirty seconds, with a 10-second pause in between.23 In conditions 3 & 4, a foam mat with the same markings as the firm surface was placed on top of the force plate. This let the person put his feet back where they were supposed to be. 25 The total Sway index was calculated for each trial and each condition average. The Sway Index is a measure of the degree of instability in addition the possibility of a fall.25
Interventions Biodex balance training
The Biodex balance system TM SD is a distinctive system that features a moveable balancing platform that can be adjusted to varying degrees of instability. Three distinct training modules were utilised to implement the LOS, maze, as well as random control training modes in this study. They were applied to enhance postural stability, postural sway control, and sensory-motor skills.22,26 All exercise modes were executed for about 30 min during each session. This session was conducted twice per week for a period of six weeks. 26 First, the patients performed in a five-minute warm-up exercise that involved brisk walking.27 Plate stability was set to 8 during the first 2 sessions by adjusting the platform's stability level.
Subsequently, the stability of the plates was diminished by one level after every two sessions. Every session involved performing each of these exercise modalities twice.26 During the LOS Training, the individual attempted to execute a movement pattern that aligned with the sway envelope, which refers to the region within which the patient has the ability to adjust their COG while maintaining their BOS.
With the pointer visible on the system's screen, they attempted to hit one of the targets that had shown before turning around to keep their balance.28 While utilising the maze control mode, the individual tried to manipulate the pointer towards maze-like targets by adhering to a consistent and predictable pattern of movement on the screen. Furthermore, the patients engaged in the random control training mode as they completed neuromuscular control tasks that involved randomly generated patterns on the display. The patient was asked to push the cursor inside the randomly shifting targets while maintaining it inside their comfort zone.29
Core stability exercises
Group A were given 24 sessions of CSE, there are eight sessions in each phase. In addition to conventional physiotherapy, three sessions are conducted on alternate days each week. Three phases were implemented during the exercise program. 30. Phase (1) consisted of abdominal bracing, single knee to chest, as well as bridging exercises. Phase (2) consisted of abdominal strengthening, basic stabilization as well as wall squats with swiss ball. Phase (3) consisted of lumbar extensor strengthening, lumbar extension on ball as well as corner stretch.31
Stretching and Strengthening Exercise
The erector spinae, illiopsoas, hamstring, along with hip adductor muscles were stretched individually on each participant in this group.32 Throughout weeks one and two, each stretch was maintained for a duration of ten seconds, with a total of five repeats. In weeks three to five, the stretches were extended to ten seconds each, with a total of ten repetitions. Finally, in weeks six to eight of the study, the stretches were held for twenty seconds each, with a total of twenty repetitions. 33
The control group's strength exercise programme consists of resistance exercise, This is performed on either a mat or using a gym ball. During a 12-week period, every participant in the exercise groups participated in two 50-minute exercise sessions each week. Throughout the duration of the exercise session, the subject was instructed to maintain a moderate to some what intense level of effort (rate of perceived exertion, (11–16). 33 (Table 1) display the comprehensive work out plans for both strength training and combining exercises.
| Group | Order | Contents | Set | RPE |
|---|---|---|---|---|
| SEG | Warm-up (10 min) | Stretching | - | - |
| Strength training (30 min) | Bridge Plank Squat Push-ups Back extension |
3–5 | 11–16 | |
| Cool-down (10 min) | Stretching | - | - |
SEG, strength exercise group; RPE, rate of perceived exertion.
Data collection
The data underwent screening to assess normality as well as homogeneity of variance. The Shapiro-Wilk test was employed to assess the normality of the data. The test demonstrated that the data followed a normal distribution (P>0.05) after removing outliers that were identified using box as well as whisker plots. Furthermore, the Levene's test utilized to assess the homogeneity of variance indicated that there was no statistically substantial distinction (P>0.05). The data exhibits a normal distribution, in addition parametric analysis is carried out.
Statistical analysis
The SPSS Package programme version 25 for Windows (SPSS, Inc., Chicago, IL) was employed to carry out the statistical evaluation. Quantitative data for clinical general characteristics (age, weight, height, and BMI), eye open firm, eye closed firm, eye open foam, and eye closed foam variables are presented as mean and standard deviation. The frequency and percentage of the categorical variable (gender) are reported and contrasted among groups using the Chi-square test.
A mixed design 3 x 2 MANOVA test was employed, with the 1st independent variable being the tested group consisting of three levels (group A, B& C). The 2nd independent variable (within the subject factor) was the measurement of periods with two levels (pre- as well as post-treatment). The Bonferroni correction test was employed to compare the pairwise within as well as between groups of the examined variables whose P-value was substantial according to the MANOVA test. The probability of all statistical evaluation was substantial (P ≤ 0.05).
Results And Discussion
In the present investigation, 48 patients, 30 of whom were male and 18 of whom were female, were randomly assigned to three equal groups, each consisting of 16 patients.
No substantial differences (P>0.05) regarding patients age (P=0.653), weight (P=0.369), height (P=0.451), BMI (P=0.207), as well as gender (P=0.766) among groups A, B, & C (Table 2).
| Variables | Groups | P-value | ||
|---|---|---|---|---|
| Group A (n=16) | Group B (n=16) | Group C (n=16) | ||
| Age (year) | 29.94 ±6.67 | 31.19 ±4.86 | 30.06 ±6.18 | 0.653 |
| Weight (kg) | 77.00 ±7.73 | 74.44 ±9.28 | 77.69 ±11.54 | 0.369 |
| Height (cm) | 168.81 ±9.82 | 171.25 ±9.05 | 171.50 ±9.20 | 0.451 |
| BMI (Kg/cm2) | 27.10 ±4.45 | 25.40 ±2.76 | 26.48 ±4.06 | 0.207 |
| Gender (males : females) | 10 (62.50%) : 6 (37.50%) | 9 (56.25%) : 7 (43.75%) | 11 (68.75%): 5 (31.25%) | 0.766 |
Quantitative data (age, weight, height, and BMI) are reported as mean ±standard deviation and compared statistically by MANOVA test
Qualitative data (gender) are reported a frequency (percentage) and compared by Chi-square test
P-value: probability value P-value>0.05: non-significant
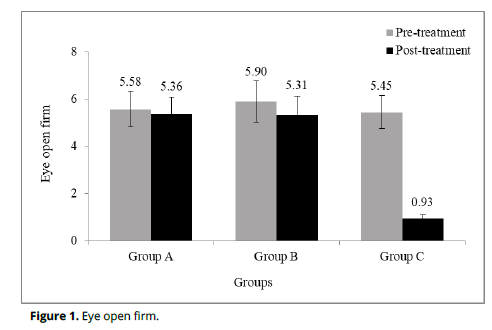
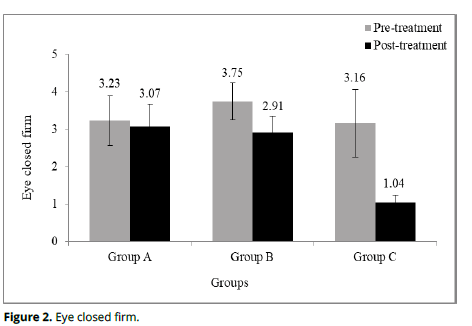
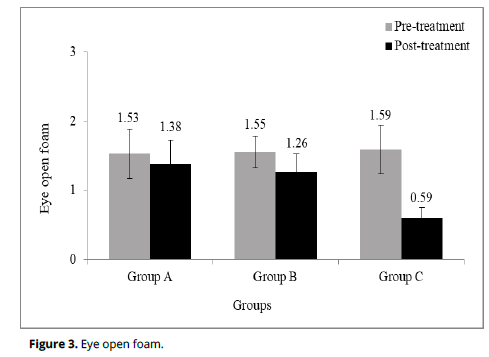
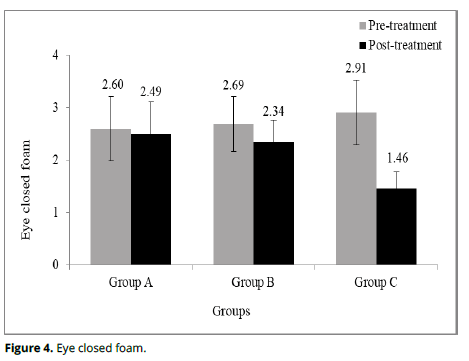
statistical evaluation within each group for main outcome variables (eye open firm, eye closed firm, eye open foam, and eye closed foam) revealed there were insignificantly (P>0.05) decreased within group A in eye open firm (P=0.395; Table 3 and Figure 1), eye closed firm (P=0.445; Table 3 and Figure 2), eye open foam (P=0.157; Table 3 and Figure 3) and eye closed foam (P=0.569; Table 3 and Figure 3) after-treatment contrasted to before-treatment. Though, there were substantially (P<0.05) decreased within group B & group C in eye open firm (P=0.022 as well as P=0.0001), eye closed firm (P=0.0001 and P=0.0001), eye open foam (P=0.007 and P=0.0001) as well as eye closed foam (P=0.048 and P=0.0001) after-treatment contrasted to before-treatment. Moreover, the patients in Group C improved higher eye open firm, eye closed firm, eye open foam, and eye closed foam (82.94, 67.09, 62.89, and 49.83%) followed by patients in group B (10.00, 22.40, 18.71, and 13.01%) and then those in group A (3.94, 4.95, 9.80, and 4.23%).
Variables |
Items | Groups (Mean ±SD) | P-value2 | ||
|---|---|---|---|---|---|
| Group A (n=16) | Group B (n=16) | Group C (n=16) | |||
| Eye open firm | Pre-treatment | 5.58 ±0.74 | 5.90 ±0.88 | 5.45 ±0.70 | 0.201 |
| Post-treatment | 5.36 ±0.71 | 5.31 ±0.82 | 0.93 ±0.17 | 0.0001* | |
| Change (MD) | 0.22 | 0.59 | 4.52 | ||
| Improvement % | 3.94% | 10.00% | 82.94% | ||
| 95% CI | -0.28 – 0.71 | 0.08 – 1.09 | 4.02 – 5.03 | ||
| P-value1 | 0.395 | 0.022* | 0.0001* | ||
| Eye closed firm | Pre-treatment | 3.23 ±0.67 | 3.75 ±0.49 | 3.16 ±0.91 | 0.395 |
| Post-treatment | 3.07 ±0.61 | 2.91 ±0.43 | 1.04 ±0.20 | 0.0001* | |
| Change (MD) | 0.16 | 0.84 | 2.12 | ||
| Improvement % | 4.95% | 22.40% | 67.09% | ||
| 95% CI | -0.58 – 0.26 | 0.41 – 1.25 | 1.69 – 2.53 | ||
| P-value1 | 0.445 | 0.0001* | 0.0001* | ||
| Eye open foam | Pre-treatment | 1.53 ±0.36 | 1.55 ±0.23 | 1.59 ±0.35 | 0.818 |
| Post-treatment | 1.38 ±0.35 | 1.26 ±0.27 | 0.59 ±0.16 | 0.0001* | |
| Change (MD) | 0.15 | 0.29 | 1 | ||
| Improvement % | 9.80% | 18.71% | 62.89% | ||
| 95% CI | -0.05 – 0.36 | 0.08 – 0.50 | 0.79 – 1.21 | ||
| P-value1 | 0.157 | 0.007* | 0.0001* | ||
| Eye closed foam | Pre-treatment | 2.60 ±0.61 | 2.69 ±0.53 | 2.91 ±0.62 | 0.253 |
| Post-treatment | 2.49 ±0.62 | 2.34 ±0.42 | 1.46 ±0.32 | 0.0001* | |
| Change (MD) | 0.11 | 0.35 | 1.45 | ||
| Improvement % | 4.23% | 13.01% | 49.83% | ||
| 95% CI | -0.26 – 0.48 | -0.02 – 0.72 | 1.06 – 1.82 | ||
| P-value1 | 0.569 | 0.048* | 0.0001* | ||
MD: Mean difference CI: Confidence interval P-value: probability value * Significant (P<0.05)
P-value1: Probability value within each group; P-value2: probability value among groups
Statistical analysis among groups for eye open firm, eye closed firm, eye open foam, and eye closed foam revealed no substantial differences (P>0.05) among 3 groups before-treatment for eye open firm (P=0.201; Table 3 and Figure 1), eye closed firm (P=0.395; Table 3 and Figure 2), eye open foam (P=0.818; Table 3 and Figure 3) and eye closed foam (P=0.253; Table 3 and Figure 3). On the other hand, there were substantial differences (P<0.05) among group A, B, as well as group C after-treatment in eye open firm (P=0.0001), eye closed firm (P=0.0001), eye open foam (P=0.0001) and eye closed foam (P=0.0001). The substantial reduction in the mean measurements for eye open firm, eye closed firm, eye open foam, as well as eye closed foam are most favourable in group C, followed by group B, and then group A (Table 3).
Post-hoc test (Table 4)revealed there were substantial differences (P<0.05) in eye open firm, eye closed firm, eye open foam, as well as eye closed foam at post-treatment among pairwise of group A vs group C (P=0.0001, P=0.0001, P=0.0001, & P=0.0001) as well as group B vs group C (P=0.0001, P=0.0001, P=0.0001, & P=0.0001). Nevertheless, no substantial differences (P>0.05) among pairwise of group A vs group B (P=1.000, P=1.000, P=0.798, & P=1.000). Group C had the highest responses for eye open foam, eye closed foam, eye closed firm, as well as eye open firm, according to the post hoc test and group means (Figure 1-4).
| Variables | Items | Post-hoc test (at post-treatment) | ||
|---|---|---|---|---|
| Group A vs. Group B | Group A vs. Group C | Group B vs. Group C | ||
| Eye open firm | MD (Change) | 0.05 | 4.43 | 4.37 |
| 95% CI | -0.56 – 0.66 | 3.81 – 5.04 | 3.76 – 4.99 | |
| P-value | 1 | 0.0001* | 0.0001* | |
| Eye closed firm | MD (Change) | 0.15 | 2.03 | 1.87 |
| 95% CI | -0.35 – 0.67 | 1.51 – 2.54 | 1.35 – 2.38 | |
| P-value | 1 | 0.0001* | 0.0001* | |
| Eye open foam | MD (Change) | 0.11 | 0.78 | 0.67 |
| 95% CI | -0.13 – 0.37 | 0.53 – 1.05 | 0.41 – 0.92 | |
| P-value | 0.798 | 0.0001* | 0.0001* | |
| Eye closed foam | MD (Change) | 0.15 | 1.02 | 0.87 |
| 95% CI | -0.31 – 0.61 | 0.56 – 1.49 | 0.41 – 1.33 | |
| P-value | 1 | 0.0001* | 0.0001* | |
CI: confidence interval * Significant (P<0.05 P-value: probability value between pairwise groups (post-hoc test)
Discussion
This investigation contrasted the effectiveness of training with the BBS and CSE on postural sway, dynamic postural stability in mechanical low back pain patients. Based on our findings, both BBS training and CSE programs appear to be beneficial for enhancing postural sway, and postural stability indices; however, BBS training appears to have a more significant impact.
Postural stability is the capacity to sustain one's position, particularly the body mass center, within specific spatial ranges referred to as the LOS. Stability limits are the spatial levels within which an individual can remain stationary without altering their degree of reliance. Many biomechanical, environmental, as well as human work-related factors influence these ranges, which are not constant. To achieve stability, one must bring the forces that produce and disturb it into balance.34 The information from each sensory tool is combined with the information from the other sensory tools to produce the proper motor response. Postural dysfunction is caused by problems with the visual, somatosensory, and vestibular systems.35
Studies using the BBS as an exercise tool in patients with MLBP are extremely rare. Hosseinifar et al. Suggested some points. First, there was a more substantial lessening in disability and pain following the implementation of stabilising activities compared to balancing trainings. Second, compared to other trainings, one type of training has a less significant effect on other research indices. Two stability indices in the balance group in addition one stability index in the stabilizing group among of the 36 studied showed differences with other groups among patients suffering from MLBP, contrary to what our study's findings that used the various Biodex assessment and treatment modalities and the literature available suggested.36
In their study, Anthony B and Piegaro Jr. found that a four-week program that combines core stabilisation and balance training can enhance semidynamic balance. On the other hand, either a core stabilization-training program or a balance training program can be utilised to enhance dynamic balance. 37
Furthermore, our study was conceptually in agreement with the findings demonstrated Beomryong K and Jongeun Y who demonstrated that both core stability as well as lumbo-pelvic-hip complex strengthening exercises enhance balance and have nearly identical effects among patients suffering from MLBP. They also observed that larger sample size studies are necessary to evaluate the impacts on both physical function as well as quality of life.38
Previous investigations have suggested that core stabilisation exercises are more effective than strengthening exercises, despite the fact that both types of exercises reduce pain. It is effective in decreasing functional disability as well as fear of movement among subjects having subacute nonspecific LBP by enhancing proprioception, balance, as well as the percentage change in transversus abdominis and lumbar multifidus muscle thickness.39
Furthermore, the meta-analysis, comprising 414 participants, revealed 5 RCTs that contrasted CSE with general exercise for chronic MLBP. The findings of this meta-analysis suggest that CSE is more effective than general exercise in providing pain relief as well as enhancing back-specific functional status throughout the Short-term duration of monitoring and evaluation.
Nevertheless, there were no substantial differences in pain alleviation during the intermediate- as well as long-term monitoring periods.40
In addition, Hicks et al. Demonstrated that stability exercise is useful in managing patients with nonspecific chronic LBP. Furthermore, lumbar stabilization programs improve the stability of the spine.41 The deep abdominal muscles, such as the superficial muscles, transversus abdominis muscle, as well as multifidus, play a crucial role in alleviating pain in the back. 42
In our study, we found that strengthening and stretching for the low back muscles, as well as BBS exercises, led to improvements in movement dynamic postural stability. In patients with MLBP, BBS training, a game-like training method, has been shown to improve dynamic balance by increasing dopamine levels and promoting more positive feelings, cognition, and motivation. 43,44 These characteristics may help to explain why the BBS training group was more effective than the core stability training group across all dynamic indices as well as postural sway.
Conclusion
From this study’s results, we conclude that both BBS training and CSE programs appear to be beneficial for enhancing postural sway, as well as postural stability indices among patients suffering with MLBP; however, BBS training is recommended for better improvement than CSE in such cases.
Ethical Considerations
This study was approved by the Ethical Committee of the Faculty of Physical Therapy, Modern University for Technology and Information (MTI) with approval number (REC/2111/MTI.PT/2112054) and it is in accordance with the Declaration of Helsinki of 1964 and its later amenamente. All participants signed consent forms for participation.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
All authors have nothing to disclose.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
The idea, design, execution, analysis, and interpretation of the study were all contributions of the authors. The final version of the Manuscript was Revised, reviewed, and approved by all authors.
References
Beeckmans N, Vermeersch A, Lysens R, et al. The presence of respiratory disorders in individuals with low back pain: a systematic review. Man Ther. 2016; 26:77-86
RD Meucci, AG Fassa and NM Faria. Prevalence of chronic low back pain: Systematic review. Rev. Saude. Publica. 2015; 49, 73.
Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord. 2017;12(1):14.
William, C, Shiel. 2012,’Low back pain overeview’,emedicine health.
Smrcina Z, Woelfel S, Burcal C. A Systematic Review of the Effectiveness of Core Stability Exercises in Patients with Non-Specific Low Back Pain. Int J Sports Phys Ther. 2022 Aug 1;17(5):766-774. doi: 10.26603/001c.37251. PMID: 35949382; PMCID: PMC9340836.
KUCZYŃSKI M., SZYMAŃSKA M., BIEĆ E., Dual-task effect on postural control in high-level competitive dancers, J. Sports Sci.,2011, 29(5), 539–545.
AKUTHOTA V., FERREIRO A., MOORE T., FREDERICSON M., Core stability exercise principles, Curr. Sports Med. Rep., 2008, 7(1), 39–44.
Y Ivanenko and VS Gurfinkel. Human postural control. Front. Neurosci. 2018; 12, 171.
Gamble K, Chiu A, Peiris C. Core Stability Exercises in Addition to Usual Care Physiotherapy Improve Stability and Balance After Stroke: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil. 2021 Apr;102(4):762-775. doi: 10.1016/j.apmr.2020.09.388. Epub 2020 Oct 22. PMID: 33239203.
Puntumetakul R, Chalermsan R, Hlaing SS, Tapanya W, Saiklang P, Boucaut R. The effect of core stabilization exercise on lumbar joint position sense in patients with subacute non-specific low back pain: a randomized controlled trial. J Phys Ther Sci. 2018;30(11):1390-1395.
ANDERSON K., BEHM D.G., The impact of instability resistance training on balance and stability, Sports Med., 2005, 35(1),43–53.
Bolarinde S.O, Adegoke, B.O.A, Ayanniyi, O., Olagbegi, O.M. Effects of Stretching Exercises on Pain and Functional Disability in Quarry Workers with Work-related Low Back Pain, J Health & Safety Research & Practice 9(2), 3-11(2017).
Hlaing, S.S., Puntumetakul, R., Khine, E.E. et al. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord 22, 998 (2021).
Sherafat S, Salavati M, Ebrahimi Takamjani I, Akhbari B, Mohammadirad S, Mazaheri M, Negahban H. Intrasession and intersession reliability of postural control in participants with and without nonspecific low back pain using the Biodex Balance System. J Manipulative Physiol Ther. 2013 Feb;36(2):111-8. doi: 10.1016/j.jmpt.2012.12.005. PMID: 23499146.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988; 15: 183340.
Amundsen PA, Evans DW, Rajendran D, Bright P, Bjørkli T, Eldridge S, Buchbinder R, Underwood M, Froud R. Inclusion and exclusion criteria used in non-specific low back pain trials: a review of randomised controlled trials published between 2006 and 2012. BMC Musculoskelet Disord. 2018 Apr 12;19(1):113.
da Silva T, Mills K, Brown BT, Pocovi N, de Campos T, Maher C, Hancock MJ. Recurrence of low back pain is common: a prospective inception cohort study. J Physiother. 2019 Jul;65(3):159-165. doi: 10.1016/j.jphys.2019.04.010. Epub 2019 Jun 14.
Madhuri G, Kunjal P. A study To Determine the Association of Body Mass Index with Performance Based Measures of Balance and Mobility in Young Adults. International journal of physiotherapy and research 2015;4(3): 1175-1179
Gribble P, Delahunt E, Bleakley C, Caulfield B, Docherty C, Fourchet F, et al. Selection Criteria for Patients with Chronic Ankle Instability in Controlled Research: A Position Statement of the International Ankle Consortium. Journal of Orthopaedic& Sports Physical Therapy 2013;43(8):585–591.
Shin J, Lee J, Kim M, Shin B, Lee M, Ha I. The long-term course of patients undergoing alternative and integrative therapy for lumbar disc herniation: 3-year results of a prospective observational study. BMJ Open. 2014;4:e005801.
Hinman M. Factor is affecting reliability of the biodex balance system: A summary of four studies. Journal of Sport Rehabilitation 2000; 9(3): 240.
Dawson N, Dzurino D, Karleskint M, Tucker J. Examining the reliability, correlation, and validity of commonly used assessment tools to measure balance. Health Science Reports 2018 ;1(12):98.
Haran F, Keshner E. Sensory reweighting as a method of balance training for labyrinthine loss. J NeurolPhysTher: JNPT. 2008;32(4):186‐191.
Antoniadou E, Kalivioti X, Stolakis K, Koloniari A, Megas P, Tyllianakis M, et al., Reliability and validity of the m-CTSIB dynamic platform test to assess balance in a population of older women living in the community. Journal of Musculoskeletal & Neuronal Interactions 2020; 20(2):185-193.
Goble D, Brar H, Brown E, Marks C, Baweja H. Normative data for the Balance Tracking System modified Clinical Test of Sensory Integration and Balance Protocol. Med Devices (Auckl).2019;12:183– 191.
SalsabiliH, Bahrpeyma F, Forogh B, Rajabali S. Dynamic stability training improves standing balance control in neuropathic patients with type 2 diabetes. The Journal of Rehabilitation Research and Development 2011; 48(7):775.
Gusi N, Carmelo A, Corzo H, Pozo B, Olivares P, Parraca J. Balance training reduces fear of falling and improves dynamic balance and isometric strength in institutionalised older people: a randomised trial. Journal of Physiotherapy 2012; 58(2):97–104.
13.Didier J, Glave A, Sarah J, Browning S, Fiaud V, Weatherwax J. Reliability of BBS LOS Test at Two Time Points in A Healthy Population. Journal of Fitness Research 2014;3(3):3-7.
Kara B, Kahraman T, Tomruk M, Çolakoğlu B, Küsbeci O. The Effects of a Postural Balance Training Program on Balance, Gait and Health-Related Quality of Life in Patients with Essential Tremor. Turk J Neurol 2018;24(1):43-48.
McGill, S. M. 2001,’ Low Back Stability’, Performance and rehabilitation. Exercise andSportScienceReviews. Vol 17, 26-31.
Narain A.Singh J.Bhowmik S. To Compare the Effect of Core Stability Exercises and Muscle Energy Techniques on Low Back Pain Patients. IOSR Journal of Sports and Physical Education (2013) 1(2) 09-15.
17.Akuthota V, Nadler SF. 2004. Core strengthening. Archives Physical Medicine Rehabilitation 85.3:86-92.
Bolarinde SAdegoke BAyanniyi OOlagbegi O. Effects of Stretching Exercises on Pain and Functional Disability in Quarry Workers with Work-related Low Back Pain. Journal of Health and Safety, Research and Practice (2017) 9(2) 1-11.
Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction of balance. Suggestion from the field. Phys Ther. 1986; 66:1548–50.
Ghez C. Posture. In: Kandel ER, Schwartz JH, Jessel TM, editors. Principles of Neural Science. 3rd ed. New York: Elsevier; 1991. pp. 596–607.
Hosseinifar M, Akbari A, Mahdavi M, Rahmati M. Comparison of balance and stabilizing trainings on balance indices in patients suffering from nonspecific chronic low back pain. J Adv Pharm Technol Res. 2018 Apr-Jun;9(2):44-50.
Piegaro, Anthony, B. Jr., "The comparative effects of four-week core stabilization and balance-training programs on semidynamic and dynamic balance." (2003). Graduate Theses, Dissertations, and Problem Reports. 10698.
Kim B, Yim J. Core Stability and Hip Exercises Improve Physical Function and Activity in Patients with Non-Specific Low Back Pain: A Randomized Controlled Trial. Tohoku J Exp Med. 2020 Jul;251(3):193-206.
Hlaing, S.S., Puntumetakul, R., Khine, E.E. et al. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord 22, 998 (2021).
Xue-Qiang Wang, Jie-Jiao Zheng and Zhuo-Wei Yu et al. A Meta-Analysis of Core Stability Exercise versus General Exercise for Chronic Low Back Pain. PLoS ONE. 2012. Vol. 7(12). DOI: 10.1371/journal.pone.0052082
Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005; 86:1753–1762
Amit K, Manish G, Taruna K. Effect of trunk muscles stabilization exercises and general exercises on pain in recurrent nonspecific low back ache. Int Res J Med Sci. 2013; 1:23–26.
Lin YT, Lee WC and Hsieh RL. Active video games for knee osteoarthritis improve mobility but not WOMAC score: a randomized controlled trial. Ann Phys Rehabil Med. 2020; 63: 458–465.
Koepp MJ, Gunn RN, Lawrence AD, et al. Evidence for striatal dopamine release during a video game. Nature. 1998; 393: 266–268.