Research Article - (2024) Volume 19, Issue 3
EFFECT OF RECIPROCAL ELECTRICAL STIMULATION VERSUS KINESIO TAPING ON FINE MOTOR SKILLS IN HEMIPARETIC CEREBRAL PALSY CHILDREN
Engi E. Sarhan1, Mohamed Bedair Ibrahim2, Basma Elsaid Mahmoud Bakr3*, Abdelsattar Abdullah Elsayeh4, Hajer M. Abdullatif5, Sally Mosad Kamar6 and Nesma EM. Barakat7*Correspondence: Basma Elsaid Mahmoud Bakr, Outpatient Clinic of Faculty of Physical Therapy, Kafrelsheikh University, Kafr Elsheikh, Egypt, Email:
2Department of Physical Therapy for Pediatrics Faculty of Physical Therapy Kafrelsheikh University, Kafr Elsheikh, Egypt
3Outpatient Clinic of Faculty of Physical Therapy, Kafrelsheikh University, Kafr Elsheikh, Egypt
4Neuropediatric Unit Faculty of Medicine Al- Azhar University, Cairo, Egypt
5Department Of Physical Therapy for Neurology and Neurosurgery, Faculty of Physical Therapy Sainai University, Kantara, Egypt
6Department of Physical Therapy for Integumentary Disorders, Faculty of Physical Therapy, Kafrelsheikh University, Kafr Elsheikh, Egypt
7Department Of Physical Therapy for Neurology and Its Surgery, Faculty of Physical Therapy, Kafrelsheikh University, Kafr Elsheikh, Egypt
Received: 11-Jun-2024 Published: 26-Jun-2024
Abstract
Background and Purpose: Cerebral palsy is a non-progressive brain lesion, which causes severe hand impairment in children with hemiparetic cerebral palsy as well. In this study, we aimed to compare the effect of Reciprocal Electrical Stimulation (RES) versus Kinesio Taping (KT) on fine motor skills in children with hemiparetic cerebral palsy.
Materials and Methods: Sixty children of either sex aged 4-5 years having hand spasticity were selected for inclusion based on a modified Ashworth scale grade between 1 to 1+.They were randomly assigned into two equivalent groups (Groups I and II).In group I, RES targeting wrist flexors and extensors was used with an individualized physical therapy program while in group II KT was applied at the wrist flexors and extensors plus the same physical treatment as in group I had. Before evaluating the Peabody Developmental Motor Scale-2 (PDMS-2), grasping and visual motor integration subtests were measured at baseline and after 12 weeks of intervention.
Results: There were no significant differences between the two groups before treatment regarding mean values of all parameters (p > 0.05). Nonetheless, it was statistically significant that Group I attained higher results than Group II after the intervention period (p < 0.05).
Conclusion: both Reciprocal Electrical Stimulation (RES) and Kinesio Taping (KT) were effective in improving fine motor skills among children with hemiparetic cerebral palsy although RES was much more effective.
Keywords
Cerebral Palsy, Hemiparetic, Electrical stimulation, Kinesio Taping.
Introduction
Cerebral palsy (CP) comprises a group of enduring movement and posture disorders arising from non-progressive abnormalities in the developing nervous system (1). The condition is estimated to occur in about two or three live births per 1,000 with 80% having spasticity. This spasticity is further classified as either quadriplegia, diplegia or hemiplegia depending on which limb it affects (2). It is interesting to note that the upper body is more affected than the lower body in approximately 30% of cases of hemiplegia (3). Cerebral palsy also results in such problems as contractures and limited movement due to secondary musculoskeletal complications resulting from weakness, spasticity and poor motor control (4).
Children with hemiplegic cerebral palsy exihibit unique motor patterns, especially during bimanual tasks, with major deviations observed in elbow supination-pronation and wrist extension (5). These deviations are important areas for intervention in addressing upper limb abnormalities in this population. Effective rehabilitation strategies usually involve a mix of therapeutic modalities such as physical exercise, occupational therapy, splinting, electrical stimulation and kinesio taping (6-8).
Neuromuscular electrical stimulation (NMES)is as a non-invasive technique that makes skeletal muscular contractions through peripheral nerves percutaneously stimulation. It works through definite frequencies, promoting weakened muscles, body composition, movement biomechanics, and functional mobility (9). Reciprocal electrical stimulation (RES) varies from NMES in duplicating muscle group firing patterns based on electromyographic information from healthy individuals involved in functional activities (10). RES intentions to simulate voluntary movement by arranging a rhythmic pattern of contractions in agonist and antagonist muscles, theoretically enhancing neural drive and generating beneficial spinal changes seen during motion.
Dr. Kenzo Kase in the 1970s established The Kinesio® taping technique, which employs latex-free cotton tape considered for elasticity, adhesion, and breathability (11). This technique is usually exploited to either facilitate or inhibit muscle function, enhance proprioception, excite cutaneous receptors and mechanoreceptors, support joint structures and alignment, and alleviate pain (12). In CP children, Kinesio taping has shown potential to enhance range of motion (ROM), individual finger movements, fine motor control, upper limb steadiness, and segmental position throughout activities like reaching and grasping (13).
Subsequently, this study intended to assess the influence of reciprocal electrical stimulation versus Kinesio taping on fine motor skills in children diagnosed with hemiparetic cerebral palsy.
Materials and methods
Pre-test post-test Randomized comparative trial, For 12 weeks. This study was conducted in the pediatrics Outpatient clinic of the Faculty of Physical Therapy Kafr el Sheikh University and the outpatient clinic of Al Obour Insurance Hospital from (February 2023 to October 2023).
Participants
Using G-power version 3.1.9.7 for Windows and regarding the t-test study, alpha level of 0.05, confidence interval of 80%, and effect size of 0.7 calculated from the previous study of Hamed et al. (14), the total sample size was 68 children (thirty- four in each group).
Sixty children aged between 4 and 5 years with a diagnosis of hemiparetic cerebral palsy were included in this study. children were recruited from the pediatrics Outpatient clinic; Faculty of Physical Therapy Kafrelsheikh University and the outpatient clinic of Al Obour Insurance Hospital, Abd El Salam Hafez St., Kafr El Sheikh - Kafr El-Shaikh - Egypt.
Microsoft Excel 2010 was used to produce an automated random number list, from which the subject allocation sequence was derived. The therapist who performed the assessments as an evaluator visited with the patients. The group assignment was hidden from the therapist. The patients were randomly assigned to either the RES or KT groups after completing their exams. Thus, neither the evaluator therapist nor the statistician knew who belonged in which group.
The children were allocated to two equal groups, Study Group I and Study Group II. Group I was given a program of selected physical therapy along with a program of reciprocal electrical stimulation. In addition to receiving the identical physical therapy regimen as Study Group I, Study Group II was also given kinesio taping. The following criteria were used to choose the participants.
The study's inclusion criteria encompasses specific conditions and parameters to ensure a targeted participant selection. These criteria were as follows: participants needed a confirmed medical diagnosis of spastic hemiparetic CP, which was determined by pediatricians or pediatric neurologists. Additionally, the children were required to have spasticity grades ranging from 1 to 1+ according to the Modified Ashworth Scale (MAS) (15) recorded by three assessors. The age range for inclusion was between 4 to 5 years, and the ability to recognize and follow verbal orders and commands during both testing and training techniques was essential.
Conversely, exclusion criteria were established to maintain the study's focus and prevent confounding variables. Individuals were excluded from participation if they presented with permanent hand deformities, visual or auditory impairments, or an intelligence quotient below 70. Additionally, those who had undergone previous surgical intervention or received Botox injections within the preceding 6 months were not included.
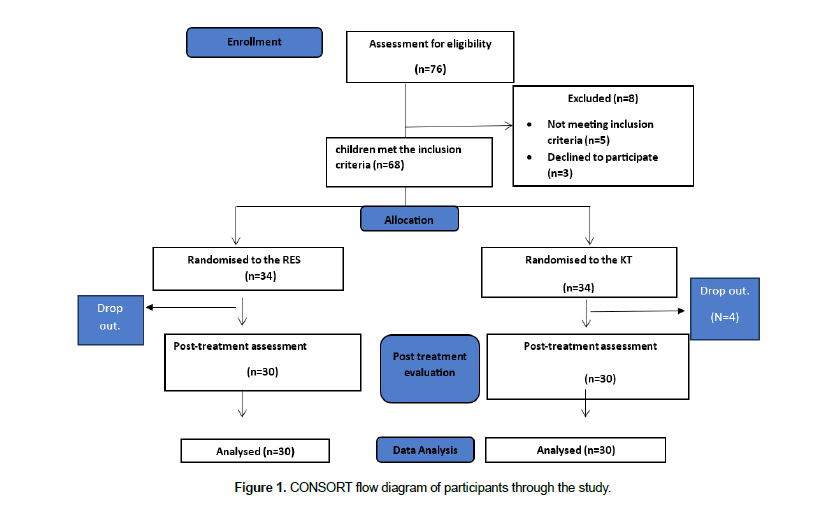
The study involved the enrollment of sixty-eight children who were randomized into two groups: RES and KT. Of these, three experienced allergic responses, and five did not finish the sessions or the final assessment (Figure 1).
This study, conducted at the Faculty of Physical Therapy, Kafr Elsheikh University, received approval from the Ethics Committee (P.T/PED/1/2023/28). To ensure transparency and adherence to ethical standards, the study's nature and objectives were comprehensively explained to all parents of the participating children. Prior to their involvement, documented consent forms were provided and signed by the parents, granting permission for their children's participation in the study. In addition, this study was officially registered and recorded on clinicaltrials.gov under the identifier number NCT05799703.
Instrumentation
The PDMS-2 test manuals' advices designed for testing environments were followed. The rooms lights were well, from overhead so no shadows were created as the child marks on paper. Free of disturbances. Each child dresses in comfortable wear. Each child sat on a chair with feet resting on the ground in front of a table wide enough and of suitable height opposite to the therapist's side. All materials used were within the reach of the assessor and outside the child's sight (16).
The PDMS-2 is a valid and reliable test to assess the motor skills in children from birth through 5 years of age (17).
Rattle, pellets, cubes, button strips, Books with thick covers and thick pages, pegboard and pegs, scissors, papers, pencils and markers, and bottles with screw-on caps were used Peabody developmental motor scale.
To stimulate the wrist flexors and extensors, a two-channel, four-electrode neuromuscular electrical stimulation device (Intelect advanced electro treatment system, model 2773MS, USA- Chattanooga group) that can stimulate two opposing groups of muscles alternately (reciprocate) was utilized.
A Latex-free Kinesio tape made from 100% cotton fibers with an anti-allergic adhesive sheet that allows for evaporation and quick drying. These properties make it durable, long-wearable, and also water-resistant. Used for both wrist flexors and extensors (18).
Procedures
An overall of 98 items on the PDMS-2's fine motor skills assessment are divided into dual classes: grasping and visual-motor integration.
Grasping contains Twenty-six items, measuring a child's hand-use abilities. the starting point is One-handed object holding then one can advance to activities requiring the planned use of both hands' fingers.
Visual-motor integration contains seventy-two items, evaluating a child's ability to combine and apply visual perceptual skills to accomplish challenging eye-hand coordination tasks. manipulative skills like handling blocks, cups, and drawing tools, among others that require skill.
Fine motor quotient is the combination of the results of two subtests
Each item was scored as follows: 2: The child completes the task following the mastery standards. 1: While the child's performance is close to meeting the item mastery criterion, it falls short of meeting all of the requirements. 0: The youngster is unable to perform the task, refuses to try, or fails to demonstrate the developing competence. Using clinical judgment, the optimal starting point for the exam was determined by choosing items that the child performed well on. A baseline was determined when a youngster scored two on three consecutive items. The examiner would offer further details. The examiner would provide more complex items until a ceiling was reached. The ceiling was set when a youngster received a score of zero on three consecutive tasks. The raw scores for each subtest were accumulated and then transformed to a standard score for each subtest and were recorded.. Before the clinical study began, each child's degree of hand performance was established using the PDMS-2, and once the therapy program was out, each child got another assessment (16, 17).
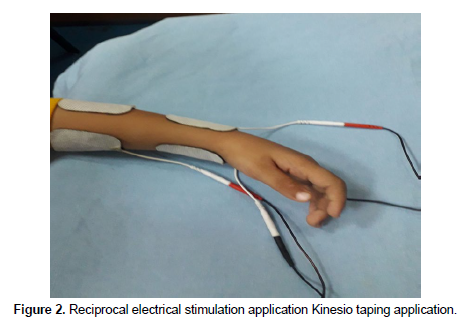
Reciprocal electrical stimulation application
As a preparation the child was positioned in a sitting position on adjustable table and chair, the arm rested on the table in a neutral position to allow free motion of the wrist in both direction. The electrodes were placed over wrist flexors and extensors after the area was cleaned with alcohol (19).
Channel 1: electrodes placed over the dorsum of the forearm as follows: one electrode was placed over the common extensor origin and the other on the back of forearm just above wrist to produce wrist extension. While Channel 2: electrodes placed on the palmar side of the forearm are as follows: one electrode was placed on common flexor origin and the other on the front of forearm just above wrist to produce wrist flexion. Figure (2) The RES was applied for a 20-minute using an asymmetrical biphasic pulsed current. The pulse duration was 300 μs (faradic), and the frequency was 5–7 pps (pulse/s), gradually increased to 30 pps . The duty cycle was set at 33%. Once a child's muscle contraction was seen, the current's intensity was adjusted based on what level the child could tolerate. Prior study on the use of electrical stimulation in cerebral palsy informed the choice of these parameters (10). Electrical stimulation was applied three sessions per week for 12 weeks (Figure 2).
Before therapeutic taping, a test piece of tension-free Kinesio Tape (two to three inches) was put. It was left on for a full day, or until the parents noted any visual or sensory skin irritation. Next, the tapped skin region was washed with water and dried or treated with an organic solvent (alcohol pad). tape was applied for six days. Following the application of tape, the skin was rested for a full day to permit skin perspiration. For a period of twelve weeks, KT was applied and removed repeatedly. Both the flexor and extensor musculature of the wrist were taped utilizing facilitatory and inhibitory kinesio taping techniques. KT was used to facilitate the extensor aspect by applying it from the origin to the insertion technique and to inhibit the flexor aspect by applying it from the insertion to the origin technique. 30% tension was applied to all the muscles for both techniques. the tape was applied from the lateral epicondyle to the base of the metacarpals covering the muscles of the dorsal aspect to facilitate muscle contraction in this muscle group. the wrist and fingers flexed, the elbow extended, and the forearm pronated. To inhibit the antagonistic muscles, tape was applied from the medial epicondyle of the humerus to the base of the metacarpals on the volar surface. The wrist was extended, the elbow was extended, and the forearm was supinated (Figure 3).
A critical physical therapy program was given to both study groups that included: neurodevelopmental program using proximal and distal key points of control. Approximation. stretching exercise for shoulder internal rotator, elbow flexors, pronators, ulnar deviators, and finger flexors to maintain length and elastic recoil. strengthening exercise to improve the functional ability of both spastic and anti-spastic muscles and gait training activities with Balance training program.
Also occupational therapy was used in the following forms: Grasping and releasing a cube, putting marbles in a wooden board or bottle, Dropping pellets, building a tower with blocks, Drinking from a cup, putting various forms in the appropriate holes, Stringing beads, Closing and opening a bottle, buttoning and unbuttoning button, playing with clay, Squeeze water out of a sponge, cutting paper into small piece, open and close zipper, Cutting paper with scissor and Writing activities: such as grasping a marker, coping a vertical line, circle, horizontal line, cross, square and connecting two dots.
Statistical analysis
The data collection process in this study involved a meticulous approach. Information was gathered through standardized assessments and measurements conducted by trained evaluators. Each participant underwent comprehensive evaluations, including functional assessments and specific measurements related to the targeted outcomes. Following data collection, a rigorous screening process was implemented to detect any missing or incomplete data points. The research team meticulously reviewed each dataset to ensure completeness and accuracy, taking necessary measures to address any inconsistencies or omissions.
To identify and address outliers, thorough checks were performed on the collected data. Various statistical methods, such as examining box plots and calculating z-scores, were utilized to detect any data points that significantly deviated from the expected range. Identified outliers were carefully reviewed to confirm their accuracy and appropriateness for inclusion in the analysis. This process ensured the reliability and integrity of the dataset by addressing any potential anomalies that could impact the study's outcomes.
Assessment of normality was conducted using the Shapiro-Wilk test within the (SPSS) version 27 for Windows.
In this study, various descriptive statistics, such as means, standard deviations, and frequencies, were employed to summarize and describe the characteristics of the collected data. For inferential analyses, T-tests were utilized to compare outcomes within and between measures, demographic variables, or different groups. Additionally, Chi-square tests were employed to assess relationships or differences between categorical variables, particularly in analyzing gender-related disparities within the study population. These statistical methods were selected based on their appropriateness for the study's objectives, providing robust analyses and meaningful interpretations of the obtained results.
Results
Upon comparing the general characteristics of subjects from both groups, it was found that there were no significant differences between the two groups in terms of mean age, height, weight, sex, and affected side (p > 0.05), as outlined in (Table 1). The values of grasping, visual motor integration and fine motor quotient of both groups within and between groups were presented and compared in (Table 2).
| Variables | Study group (I) | Study group (II) | t-value | p-value | Sig. |
|---|---|---|---|---|---|
| Age (years) | 4.83 ± 0.75 | 4.8 ± 0.76 | 0.171 | 0.865 | NS |
| Height (cm) | 100.18 ± 8.56 | 102.4 ± 6.76 | 1.114 | 0.27 | NS |
| Weight (kg) | 19.15 ± 2.45 | 19.3 ± 2.96 | 0.214 | 0.832 | NS |
| Sex (M: F) | (16: 14) | (18: 12) | 0.6 | NS | |
| Affected side (Rt: Lt) | (14: 16) | (13: 17) | 0.8 | NS |
Variables |
Study group (I) | Study group (II) | T value | P value |
|---|---|---|---|---|
| Pre grasping | 39.33 ± 2.12 | 39.67 ± 2.38 | 0.572 | 0.569 |
| Post grasping | 48.47 ± 2.1 | 45.53 ± 2.8 | 4.606 | 0.00002 |
| % of change | 23.24% | 14.77% | ||
| T value | 19.781 | 19.412 | ||
| P value | 5.3 E -17 | 3.7 E -18 | ||
| Pre VMI | 73.4 ± 10.52 | 73.2 ± 10.58 | 0.073 | 0.942 |
| Post VMI | 108.93 ± 16.24 | 97.57 ± 17.08 | 2.642 | 0.011 |
| % of change | 48.41% | 33.29% | ||
| T value | 19.074 | 12.703 | ||
| P value | 6.8 E -17 | 2.2 E -13 | ||
| Pre FMQ | 53.8 ± 2.17 | 54.1 ± 2.25 | 0.526 | 4.996 |
| Post FMQ | 80.6 ± 8.14 | 68.5 ± 10.47 | 0.601 | 5.7 E -6 |
| % of change | 49.81% | 26.62% | ||
| T value | 19.539 | 8.835 | ||
| P value | 1.1 E -16 | 1 E -9 |
Discussion
No significant differences were noted when comparing the baseline mean values of all measured variables in both groups. However, the pre-treatment mean values of grasp, visual motor integration, and fine motor quotient scores revealed a substantial decrease. This decline specified significant hand use difficulties among the children.
These results were reinforced by Basu et al.'s observations in hemiplegic cerebral palsy (CP) children, where major spasticity was notable in upper limb flexors, accompanied by weakened extensors and limited range of motion (ROM) in forearm supination and wrist extension. Such impairments precisely affect appropriate hand position and function (20) (8).
Significantly, the group undergoing reciprocal electrical stimulation (RES) showed a statistically significant improvement in grasping scores that’s relate to the effect of electrical stimulation on increasing ROM and muscle strength and reducing spasticity. A support for the benefits of RES comes from Hamed et al.'s study involving spastic hemiplegic cerebral palsy children aged 10-14 years. Their research emphasised the superiority of RES on wrist flexors and extensors combined with an exercise program in improving handgrip and pinch grip strength, attributing the positive outcomes to RES's synergistic effect in reducing cortical excitability of spastic flexors and enhancing weak extensor strength (14). According to Kamper et al., wrist extension improved after three months of NMES treatment for seven individuals with unilateral cerebral palsy, ages five to fifteen. There have also been reports of reduced stiffness and increasing active wrist extension following a 6-week NMES treatment targeted at the wrist extensors (21).
There was a significant difference in the grasping subtest raw scores in the kinesio taping group Afterward 12 weeks of treatment. The synchronised use of kinesio taping over wrist extensors and flexors may make the technique used in this study valuable. The purpose of the application of kinesio taping with this procedure was to increase the function of weak wrist extensors and decrease the tonicity of wrist flexors, by increasing local blood flow and reducing excessive tension. Facilitatory technique over wrist extensors can improve joint ROM, activate weak muscles, and support joints; the addition of inhibitory technique over wrist flexors helps in reducing muscle tone by stretching of Golgi tendon organ.
The evolving literature encompassing the effect of Kinesio taping on various motor functions and conditions emphasises its potential in prompting functional abilities. Chitaria et al. noted a pivotal development in proximal joint control between ages 4 to 6, crucial for enhancing fine motor skills of the hand. This understanding clarifies the effectiveness of kinesio taping in refining hand movements (22). In a related vein, Mehraein et al. discovered the inhibitory effect of KT application on the gastrocnemius muscle in stroke patients, successfully reducing the H max/M max ratio after 48 hours (23). Opposite results were observed in a pilot study involving 11 hemiparetic cerebral palsy children, wherein Kinesio taping applied to the wrist and thumb for four weeks didn't yield changes in grasping subtest scores of upper extremity skills or Peabody developmental motor scale. This discrepancy may be attributed to the short-term intervention duration (24).
There were statistically significant difference in the visual motor integration subtest scores in the RES group that may be attributed to the effect of ES in restoring the normal movement pattern by improving the coordination between wrist flexors and extensors muscles and proper motor control.
The findings are consistent with those of Xu et al. (2012), who studied the effects of adding electrical stimulation to constraint therapy in children with hemiplegia between the ages of 2 and 14 years. The results demonstrated a significantly higher percentage of improvement in the VMI subtest of PDMS at 3 and 6 months of treatment compared to either constraint or occupational therapy alone (P<0.05). This may be attributed to the way in which ES strengthens the wrist muscles by increasing their cross sectional area and selectively recruiting type 2 muscle fibers, which improves the muscle's synaptic efficacy and reduces muscle tone (25).
Also significant improvement was observed VMI subtest raw scores in in the kinesio taping group, as the combined application on both wrist group muscles provide proximal joint control this lead to improving functional control at thumb and fingers.
In a quasi-experimental study the kinesio taping was applied for 3 days, marginal increase of raw and percentile scores of VMI subtest was found, but these changes were not significant in age equivalent that may be attributed to the short period of application (26).
Following the intervention, the fine motor quotient of the children in the RES group considerably improved (p<0.01). With early intervention, preschool-aged children may make quick progress in their acquisition of hand function, which could account for this notable improvement. Moreover, rather than completing isolated tasks, the results show how the program of exercise that was selected improved hand function from a functional position. The use of RES in addition to exercise program helps children to practice the normal movement pattern and the best functional position. This coincides with Chasiotis et al.'s 2022 report, supporting the usefulness of electrical stimulation in reducing post-stroke spasticity and boosting overall performance, whether applied to spastic or non-spastic muscles, alone or in concurrence with physical therapy programs (27).
Additionally, Elnaggar et al.'s 2020 results highlighted a prominent improvement in upper limb function between spastic hemiplegic children in the reciprocal neuromuscular electrical stimulation group, mostly when used combined with botulinum neurotoxin-A (28). Additional evidence from Badawy and Ibrahim in 2015 highlighted the beneficial effects of RES on knee extensors and flexors in improving postural dysfunction in diplegic children. The attributed explanation for these findings lies in repetitive cyclic stimulation aiding in modifying the co-activation of agonist and antagonist muscles toward a near-normal pattern (10).
Likewise, fine motor quotient scores revealed statistically significant improvement in the KT group(P<0.01), that may be attributed to the effect of KT in improving balance between wrist flexor muscles (spastic) and wrist extensor muscles (weak) and modulating the normal posture of hand . KT application for CP children helps in muscular facilitation or inhibition, joint realignment, mproving proprioception and postural suooprt. KT also activates skin mechanoreceptors by applying pressure and stretching; this activation could result from physiological modifications such as increased firing in muscle recruitment patterns (29).
Tabatabaee et al.'s study on Kinesio taping application for lower limb spastic and anti-spastic muscles in CP patients demonstrated improved range of motion, functional mobility, and reduced spasticity after 2 weeks, a change not observed within 2 days (30). Kora et al. in 2018 conducted a comparative analysis of inhibitory and facilitatory kinesio taping techniques in spastic CP children, revealing a significant enhancement in gross motor quotient for both methods, aligning with our own findings (31). Çekmece et al.'s 2022 investigation into Kinesio taping's impact on wrist, finger, and thumb extension ranges, specifically in hemiplegic cerebral palsy children, showcased its effectiveness in enhancing hand function using facilitatory techniques (32). Conversely, Murugan et al. in 2021 didn't find significant changes in spasticity, range of motion, or hand function in chronic stroke patients after a 48-hour application of KT on wrist flexors and extensors, except for immediate improvements in handgrip strength, likely due to the brief treatment duration (33). A 2023 Randomized trial assessing the impact of KT combined with an exercise regimen involving functional hand activities found that children with cerebral palsy did not see an improvement in hand function (34).
Comparing the post treatment means of all measured variables of both groups showed significant improvement in favor to the RES group. These findings come in agreement with Karabay et.al. who reported that neuromuscular electrical stimulation application for 4 weeks was more effective than KT in improving trunk and posture control in children with cerebral palsy (35).
In a study comparing the consequences of electrical stimulation and KT upon hand extensors, significant differences between groups were observed in the unilateral Minnesota Hand Skill Test, left shoulder abduction, and left shoulder flexion in favor of NMES. In contrast, Kinesio taping was found to be beneficial for a considerable improvement of left elbow flexion (36).
The study encountered several limitations that warrant consideration. Firstly, it lacked a control group, which hindered the ability to compare outcomes against a baseline or alternative intervention. Secondly, the scope of the study was confined to children with 1 and 1+ MAS, potentially limiting the generalizability of the findings to a broader population. Furthermore, employing tests like electromyography could have offered an objective measurement of the effects of Kinesio Taping (KT) and reciprocal electrical stimulation (RES). Lastly, a notable drawback was the absence of a cost analysis pertaining to the utilization of kinesio taping throughout the duration of the study. These limitations underscore areas for potential improvement in future research endeavors, aiming to enhance the comprehensiveness and applicability of the findings.
Conclusion
The ground-breaking study investigated the impact of combining Reciprocal Electrical Stimulation and Kinesio Taping on the fine motor skills of children with hemiparetic cerebral palsy (CP). Incorporating both techniques into the conventional physical exercise regimen demonstrated notable enhancements in fine motor skills. This improvement was attributed to the concurrent increase in muscle strength and reduction in spasticity.
The integration of Reciprocal Electrical Stimulation and Kinesio Taping alongside traditional physical exercises presents a promising avenue for enhancing fine motor skills in children with hemiparetic CP, potentially offering more comprehensive therapeutic approaches for managing motor impairments.
Future research endeavors could delve deeper into exploring the long-term effects and optimal implementation strategies of combining Reciprocal Electrical Stimulation and Kinesio Taping within rehabilitation programs for individuals with hemiparetic CP. Additionally, investigating the potential impact on other aspects of motor function and quality of life in a larger sample size could further broaden our understanding and therapeutic applications in this population.
Acknowledgements
The family members and children who agreed to engage in the study are appreciated by the authors.
Conflict of interests
The authors declare no conflict of interest.
Funding
No funding
References
Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: Current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505–18.
Korzeniewski SJ, Slaughter J, Lenski M, Haak P, Paneth N. The complex aetiology of cerebral palsy. Nat Rev Neurol [Internet]. 2018;14(9):528–43. Available from: http://dx.doi.org/10.1038/s41582-018-0043-6
Vitrikas K, Dalton H, Grant D. Cerebral Palsy: An Overwiev. Am Fam Physician [Internet]. 2020;101(4):213–20. Available from: https://pubmed.ncbi.nlm.nih.gov/32053326/
Veruggio G. Upper Limbs Functional Problems in Different Forms of Cerebral Palsy. Cerebral Palsy. 2022. 309–370 p.
Santos CA, De Moura RCF, Lazzari RD, Dumont AJL, Braun LAF, Oliveira CS. Upper limb function evaluation scales for individuals with cerebral palsy: A systematic review. J Phys Ther Sci. 2015;27(5):1617–20.
Cacioppo M, Lempereur M, Marin A, Rauscent H, Crétual A, Brochard S, et al. Motor patterns of the impaired upper limb in children with unilateral cerebral palsy performing bimanual tasks. Clin Biomech. 2022;97.
Mohamed SS, Ghany WAA, Abdelazeim FH. Upper limb physical therapy interventions to improve functions in cerebral palsy children: A review article. Int J Health Sci (Qassim). 2022;(September):6545–60.
Basu AP, Pearse J, Kelly S, Wisher V, Kisler J. Early intervention to improve hand function in hemiplegic cerebral palsy. Front Neurol. 2015;5(January):1–9.
Chen YH, Wang HY, Liao C De, Liou TH, Escorpizo R, Chen HC. Effectiveness of neuromuscular electrical stimulation in improving mobility in children with cerebral palsy: A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2023;37(1):3–16.
Badawya WM, Ibrahimb MB. Balance training versus reciprocal electrical stimulation on knee joint alignment in spastic diplegic cerebral palsy children. Bull Fac Phys Ther. 2015;20(2):146–53.
Cavalcante JGT, Silva MDC, Silva JTDF, dos Anjos CC, Soutinho RSR. Effect of Kinesio Taping on Hand Function in Hemiparetic Patients. World J Neurosci. 2018;8(2):293–302.
Setiawati E. The Effect of Wrist Kinesiotaping on Hand Motor Exercise in Fine Motor Skill for Children with Cerebral Palsy. Indones J Phys Med Rehabil. 1970;10(1):1–10.
El-Karim MAEFA, El-Wahab MSA, Ibrahim NM. Kinesiotaping versus Wrist Wheel on Upper Extremity Functions in Children with Unilateral Cerebral Palsy. Egypt J Hosp Med. 2022;89(2):6839–44.
Hamed AE, El-Din Taha TS and Matty SM (2021). The effect of reciprocal electrical stimulation on handgrip and pinch grip strength in spastic hemiplegic cerebral palsy child. J Med Sci Res, 4, Pp. 282-288.
Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206–7.
Connolly BH, McClune NO, Gatlin R. Concurrent validity of the bayley-III and the peabody developmental motor scale-2. Pediatr Phys Ther. 2012;24(4):345–52.
Zanella LW, Valentini NC, Copetti F, Nobre GC. Peabody Developmental Motor Scales - Second Edition (PDMS-2): Reliability, content and construct validity evidence for Brazilian children. Res Dev Disabil. 2021;111.
Kase K, Wallis J and Kase T. Clinical therapeutic applications of the Kinesio taping method. 2nd ed. Tokyo: Ken Ikai; 2003
Bellew JW, Michlovitz SL, Nolan Jr TP. Michlovitz's modalities for therapeutic intervention. FA Davis; 2016 Apr 21.
Goyal C, Vardhan V, Naqvi W. Virtual Reality-Based Intervention for Enhancing Upper Extremity Function in Children With Hemiplegic Cerebral Palsy: A Literature Review. Cureus. 2022;14(1):1–7.
Kamper DG, Yasukawa AM, Barrett KM, Gaebler-Spira DJ. Effects of neuromuscular elec- trical stimulation treatment of cerebral palsy on potential impairment mechanisms: a pilot study. Pediatr Phys Ther 2006; 18: 31–8.
Chitaria SB, Narayan A, Ganesan S. Short- term effects of kinesiotaping on fine motor function in children with cerebral palsy-a quasi-experimental study. Crit Rev Phys Rehabil Med 2015; 27(1): 41-50.
Mehraein M, Rojhani- Shirazi Z, Zeinali Ghotrom A, Salehi Dehno N. Effect of inhibitory kinesiotaping on spasticity in patients with chronic stroke: a randomized controlled pilot trial. Top Stroke Rehabil. 2022;29(8).
ELHAM E. SALEM, Ph.D. AAZEDMS., KAMEL H. MORSY, M.D. SESPD. Effect of Kinesio Taping on Grasp and Release in Children with Spastic Hemiparetic Cerebral Palsy: A Pilot Study. Med J Cairo Univ. 2018;86(9):2177–84.
Xu K, Wang L, Mai J, He L: Efficacy of constraint-induced movement therapy and electrical stimulation on hand function of children with hemiplegic cerebral palsy: a controlled clinical trial. Disabil Rehabil 2012, 34:337–346
Erna Setiawati. The Effect of Wrist Kinesiotaping on Hand Motor Exercise in Fine Motor Skill for Children with Cerebral Palsy. Indones J Phys Med Rehabil. 1970;10(01):1–10.
Chasiotis A, Giannopapas V, Papadopoulou M, Chondrogianni M, Stasinopoulos D, Giannopoulos S, et al. The Effect of Neuromuscular Electrical Nerve Stimulation in the Management of Post-stroke Spasticity: A Scoping Review. Cureus. 2022;14(11):3–9.
Elnaggar RK, Alqahtani BA, Elbanna MF. Functional outcomes of botulinum neurotoxin-A injection followed by reciprocal electrical stimulation in children with cerebral palsy: A randomized controlled trial. Restor Neurol Neurosci. 2020;38(6):431–41.
Allah Rastil Z, Shamsoddini A, Dalvand H, Labaf S. The effect of Kinesio taping on handgrip and active range of motion of hand in children with cerebral palsy. Iran J Child Neurol. 2017;11(4):43–51.
Kashoo FZ, Ahmad M. Comment to “The effects of Kinesio taping of lower limbs on functional mobility, spasticity, and range of motion of children with spastic cerebral palsy” by Mirjavad Tabatabaee et al. Egypt J Neurol Psychiatry Neurosurg. 2020;56(1):4–9.
Kora A, Abdelazeim F, Olama K, Raouf E, Abdelraouf O. Muscle Inhibitory Vs Functional Corrective Kinesio Taping on Gross Motor Functional Abilities in Children with Spastic Cerebral Palsy. J Complement Altern Med Res. 2018;6(1):1–9.
ÇEKMECE Ç, SADE I, İNANIR M, DURSUN N, SELÇUK B, DURSUN E. The Effect of Kinesiologic Taping on Hand Function in Children With Cerebral Palsy. Kocaeli Üniversitesi Sağlık Bilim Derg. 2022;8(2):144–8.
Murugan S. Does Kinesio Taping Improve Handgrip Strength and Hand Function in Patients with Chronic Stroke? Int J Physiother. 2021;8(2):99–104.
James J, Javed J, Mohan D, Vasanthan R. Effect of Kinesiotaping for Hand Function in Children with Cerebral Palsy: A Randomized Controlled Trial. Indian J Physiother Occup Ther - An Int J. 2023;17(2):3–7.
Karabay I, Do˘gan A, Ekiz T, Koseo˘ glu BF, Ersoz M. Training postural control and sitting in children with cerebral palsy: Kinesio. taping vs neuromuscular electrical stimulation. Complement Ther Clin Pract. 2016 ; 24:67–72.
Acikbas E, Tarakci D, Budak M. Comparison of the effects of Kinesio tape and neuromuscular electrical stimulation on hand extensors in children with cerebral palsy. Int J Ther Rehabil. 2020;27(7):1–12.