Full Length Research Article - (2023) Volume 18, Issue 4
Effect Of Robotic-Assisted Gait Training In Pediatric Population With Incomplete Spinal Cord Injury (A Randomized Controlled Trial)
Wagdy William Amin Younan Lecturer of physical Therapy1*, Mina Nashaat Halim Lecturer of physical Therapy2, Nadia Mohamed Abdelhakiem Lecturer of Physical Therapy2, Heba S. AbdelTawab Lecturer of physical therapy, Emad Makram Ghattas Lecturer of physical therapy for integumentary diseases and its surgeries, Mohamed Hesham Abouelenein Lecturer, Basic Science Department and Safi M Mahmoud Lecturer of Pediatric physical therapy*Correspondence: Wagdy William Amin Younan, Lecturer of physical Therapy, Department of physical Therapy for disturbance of growth and development in pediatric and it is Surg, Egypt, Email:
2department of physical Therapy for internal medicine and geriatrics-Faculty of Physical Therapy,, Egypt
3Pediatric Department, Egypt
4Suez Canal University, Egypt
5Basic Science Department, Misr University for Science and Technology, Egypt, Misr University for Science and Technology, Egypt
6Lecturer of Pediatric physical therapy Department, Jordan
Received: 07-Aug-2023 Accepted: 21-Aug-2023 Published: 21-Aug-2023
Abstract
Background: The ability to walk again is often lost following a spinal cord injury (SCI), making it one of the most important goals for patients. In the last decade, robotic-assisted gait training has become a prominent rehabilitation therapy for enhancing people's walking patterns after neurological impairment. Objective: To evaluate the efficacy of robotic-assisted gait training (RAGT) in children having incomplete spinal cord injury compared to traditional rehabilitation training. Methods: Thirty patients having motor incomplete spinal cord injury (SCI), aged 7-14, were recruited and randomly assigned to two groups in a specialized rehabilitation institution (15 children each). The Control Group (CG) participated in conventional therapy for 1 hour per day, 5 days per week for a whole month, whereas the Study Group (SG) underwent RAGT in addition to conventional physiotherapy on the following schedule: 3 days with RAGT& 2 days with regular treatment a week for 1 month. Main outcome measures: Biodex isokinetic dynamometer & walking index used for spinal cord injury version II (WISCI-II) were performed before and after the intervention to provide indicators for improvement in ambulatory and decrease in patients' degree of impairment. Results: As compared to the control group, the study group has shown statistically substantial improvement. Conclusion: It is possible that ambulatory function can be improved by RAGT when compared to traditional physiotherapy. In children with incomplete spinal cord injuries, RAGT can be a useful adjunct to other rehabilitative methods.
Keywords
Spinal cord injuries. Robotics. Biodex isokinetic dynamometer. Walking. Rehabilitation
Introduction
The quality of life for those with spinal cord injuries (SCIs) is reduced substantially. Spinal cord injury causes paralysis of the patient's voluntary muscles, limiting the patient's mobility and independence. [1]. Motor incomplete lesions now account for more than half of all SCI patients. There has been a rise in the rate of SCIs that are partially repaired. [2]. When a spinal cord injury is partial, some function persists below the site of the initial damage. An individual with an incomplete injury may have more mobility in one arm or leg than the other, or one side of their body may continue to function normally. [3].
Within the first two months following an injury, motor function often returns to normal. Approximately 75% of those who sustain an initial motor incomplete SCI recover some degree of mobility. Patients with an impairment grade of D on the American Spinal Injury Association (ASIA) impairment scale had a very good prognosis at 12 months after injury. [4,5].
The cost of effective gait therapy for people with spinal cord injuries is unaffordable. Additionally, qualified physiotherapists who are able to take into account various aspects of the patient's physical condition are essential. Decreased sensory-motor coordination, spasticity, and decreased balance are the main obstacles that people with partial SCI face when attempting to walk over ground.[6]
Robotic-assisted gait training (lokomat) gives the child the chance to get more walking practise with mechanical help from robots instead of therapists in cases where the child may not be able to make the right movement enough times to improve their gait [7].
Numerous studies afford evidence that RAGT helps motor recovery also functional improvement [8]. Moreover, RAG device has been established to diminish the physical effort as well as time of physiotherapists, also to lengthen the amount of time that gait kinematics are repeated. Patients with gait disorders are being helped by a device called RAG, which is intended to produce regular walking patterns in the patient's lower limbs.[9].
Patients walk more quickly and complete more gait cycles during RAGT than they would during traditional gait training. [10]. Lokomat training, however, is now widely regarded as a viable option for treating a variety of diseases, including but not limited to SCI, stroke, multiple sclerosis, as well as cerebral palsy, and can be incorporated into the standard therapy program. [11].
The purpose of this research was to compare robotic-assisted gait training (RAGT) to traditional training for improving ambulation and reducing impairment in children with incomplete spinal cord injury.
There is limited research studying the effect of robotic-assisted gait training (RAGT) to promote gait improvement in pediatric population with incomplete SCI and there is no research studying its intermediate effect.
Did repetitive robotic-assisted gait training (RAGT) improve patient gait patterns in pediatric population with incomplete SCI?
Materials and Methods
Study design
A pre-post-test randomized controlled trial. In accordance with the "Institutional Ethical Committee Clearance," we obtained formal permission from the children's guardians and followed their instructions. Faculty of physical therapy Cairo university research ethical committee (P.T.REC/012/0045492).
Participants
This investigation was carried out in HAVEN physical therapy center from February 2022 to October 2022 with a simple random sample. Thirty patients with motor incomplete SCI aged between 7-14 years were chosen at random from the integrated rehabilitation facility, and then divided into 2 groups of equal size (15 child each)
All participants in this Study understood and followed the verbal instructions provided. They fulfilled the following requirements for inclusion: 1) spinal cord injury that does not worsen over time due to trauma 2) the onset is within the first six months, and 3) classed via the American Spinal Injury Association (ASIA) impairment scale with grade D while enrolment. Exclusion criteria were SCI patients with autonomic dysreflexia who have sustained injuries above T6, patients having pressure sores, limited mobility in the hips and knees, profound mental impairment, or patients having pulmonary and or Patients with cardiac conditions that require close attention during training and presence of severe osteoporosis. Patients were also excluded if they had previously experienced RAGT. Before any sort of intervention was attempted, baseline measurements of the relevant outcome variables were obtained.
Randomization
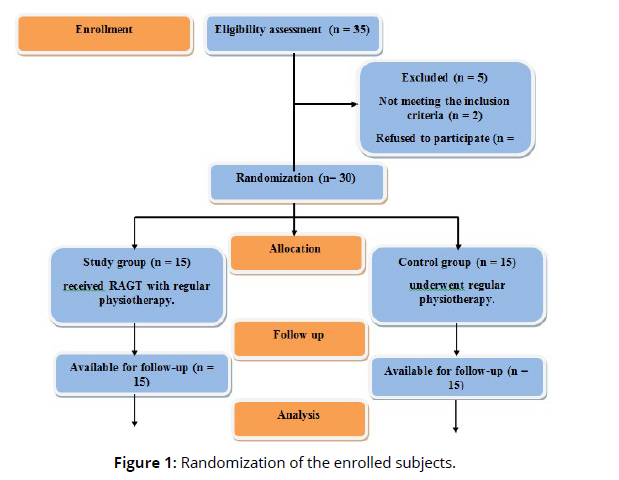
Forty-six participants were assessed for eligibility. Thirty patients who have motor incomplete SCI have been assigned as in the flowchart (Fig.1). Two groups were allocated randomly to participants. Simplified randomization was applied by generating random numbers from odd and even integers to allocate youngsters in two equal-number groups. A sheet of paper carrying a secret digit was asked to be drawn blindly from a case for each child; odd numbers were assigned to the control group while even numbers were given to the test group (Figure 1).
Intervention
Physical therapy was administered to all patients in the study within 4 weeks of their treatment. The SG underwent RAGT along with conventional physiotherapy, with RAGT administered on three days and conventional treatment on two days weekly. The total time spent on RAGT training was 1 hour, 40 minutes of which were spent on actual training. Subjects received conventional physiotherapy twice weekly for one hour per session during the rest treatment days. The CG underwent physiotherapy on a regular basis Stretching, Bobath approach, strengthening, balancing, and gait training exercises, each lasting one hour, performed five times each week.
Procedures
Assessment procedures: The assessors were blinded folded to group allocation.
Within 48 hours of the beginning and ending of the training period, all participants were evaluated.
1. The ability to walk was evaluated according to the walking index for spinal cord injury version II (WISCI-II).
The Walking Index for Spinal Cord Injury, Version 2 (WISCI-II) was a 20-item scale that evaluated the degree of physical assistance, braces or devices needed to walk 10 metres after a spinal cord injury.
For WISCI-II a score between 0 and 20 is given. Level 0 "patient is unable to stand and /or participate in walking" to 20 " ambulate with no devices and no assistance.
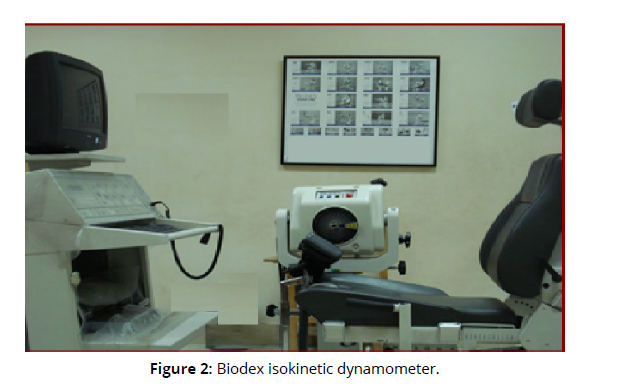
2. Biodex isokinetic dynamometer
The Biodex system, one of the most extensive computer-driven, biomechanical musculoskeletal assessment & rehabilitation with 3 pro multi-joint systems, was used to measure the isokinetic function of the quadriceps & hamstring muscles of all patients (Biodex medical system, Shirley, New York, USA). It is accessible at HAVEN physical therapy center. Subjects were given tests to determine the parameters of concentric contraction performance of the quadriceps & hamstrings. Multiple torso, shoulder, knee, & ankle attachments, as well as isolation straps, are included with the machine. The software comes with a selection of predetermined options. Input is made via a typewriterstyle keyboard into the device's central CPU. The final results are displayed graphically and/or printed out in a variety of formats, including a chart showing test data and graphs showing torque, speed, duration, movement, work, power (Figure 2).
Testing procedure
Using an isokinetic dynamometer, the following isokinetic muscular performance parameters were measured bilaterally for all children at each angular velocity. The concentric right& left isokinetic knee extensor& flexor peak torque in Newton-meters (Nm) were recorded.
a. Isokinetic set up and positioning
Isokineting initialization:
For the Biodex system to be set up, the main power, the computer power, and the dynamometer power all had to be turned on, and anything that was attached to the dynamometer had to be taken off. The shaft of the dynamometer was allowed to turn freely for a few seconds, until the system showed a message that the dynamometer had been set up. Once the automatic initialization steps were done, the system status window said to press the start key again.
Apparatus adjustment:
Before any tests were done on the system, the equipment was set up and adjusted so that it was ready to use. Before the child set the machine, the ROM was set to 90 degrees of the full range. By moving in an arc of 90 degrees, peak torque could be measured at all speeds.
Chair bench operation:
This included adjusting the height of the chair, the angle at which the back support tilted, the accessories that fit the tested knee, and the straps that held the accessories on. The back angle of the seat was positioned to 90 degrees from the horizontal, which was the most upright position. 100 degrees from the vertical was the angle of the hip when it was flexed
Fitting attachments:
From sitting position, testing the knee joint extension flexion cycle was executed for all children, the knee attachment was fixed to the power head shaft, and the axis of the power head had been in line with the axis passing through the femoral condyles in the sagittal plane. The resistance pad was placed proximal to the malleolii (above lateral malleolus by 2 fingers) and below the prominent calf musculature. Stabilization of the leg took place while still allowing full dorsiflexion at the ankle. All children were stabilized by strapping their trunks, pelvis and -thigh to the testing chair. This ensured muscle isolation and repeatability.
Isokinetic testing protocol included standardization of guidelines established by Wilk (1990) was followed. The goal of these guidelines was to improve the reproducibility of the test results [12]. The guidelines were as follows:
1. The system of calibration and stabilization were applied by the Laboratory Research Associate.
2. The procedures were explained to each child through verbal education about isokinetic and practice repetitions to make them comfortable and responding.
3. The axis of rotation was aligned for safety of the joint movement and for preventing substitution of the muscles being tested.
4. Warm-ups were allowed to let the child feel the speed of the lever arm and to apply submaximal and maximal effort at various speeds.
5. Stabilization was conducted by using straps provided on chair to prevent accessory movements of the segments.
6. The children were encouraged during testing procedures by using verbal commands and visual feedback.
7. Fast speed tests (120%sec) were selected to be used.
8. Slow speed tests (60%sec) were conducted with 5 repetitions and rest periods of less than 2 minutes between speeds.
9. The arc of range of motion for each child ranged from 90° flexion up to full extension.
b. Testing protocol
Personal data including name, age and sex was collected from each child.
The height and weight of the subjects were measured. Total body mass (in kilograms) was identified using a calibrated scale that was set to zero before each weighting. A stadiometer was used to measure body height to the nearest 0.5 cm. For both measurements, the children are told to put on light clothes, take off their shoes, stand up straight, & look straight ahead.
A musculoskeletal examination of the lower extremities was done, which included inspection, palpation, an examination of the knee's ligaments, measurements of the knee's range of motion, as well as a manual muscle test to both quadriceps femoris & hamstring muscles.
The subjects' positioning and stabilization:
1. Each child was fastened to the seat with a wide belt which held the pelvis, chest straps, as well as a horizontal pad well over middle third of the thigh, just above the knee, to stop any extra movement and otherwise substitutions that would change the measurements.
2. The subjects used the chair's side handles to further stabilize themselves and simply focus on moving their knees.
3. While testing a knee, the axis of rotation of the dynamometer was lined up with the axis of rotation of the level arm. The lever arm's resistance pad was fastened to the tibia's distal region, just above the malleoli (above lateral malleolus by 2 fingers).
4. The subject was asked to sit down before the test, and after they were comfortable, they were instructed to let their leg freely fall through its full range of motion at a constant angular velocity. The system was calibrated according to accepted practices, and all torque results were corrected for the gravity's influence on the dynamometer arm & leg's weight.
5. All of the test subjects took a preliminary test to get accustomed to the equipment and the way the test was done. Standard isokinetic knee testing consisted of one set of maximum repetitions for each knee. Slow speed (60 degrees per second) for 5 times. Fast angle speed (120 degrees per second) for 5 times.
6. Demonstration of the movement at a variety of speeds followed by sub-maximal repetitions also familiarized the child with the dynamometer, thus increasing the validity and reliability of the testing The child verbal command during testing was standardized, to move his leg in extension then into flexion with his maximal effort as fast and hard as possible. This ensured the reproducibility of the testing. The instructions were very simple to avoid any technical details and to provide examples of movements that are already known to children to help them understand what they are required to do, such as:
a. This machine measures the strength of your legs so you must try your best.
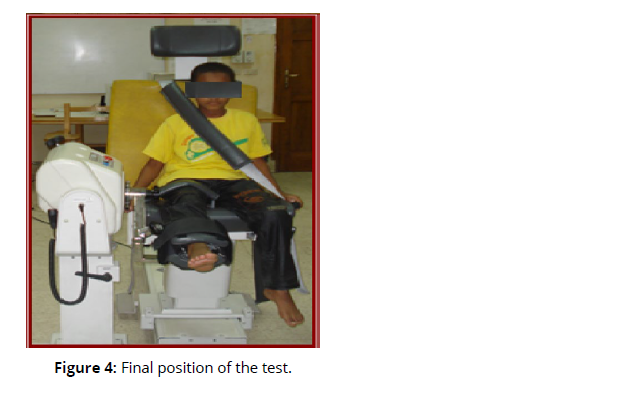
b. You must kick with your leg all the way to the end until your knee is straight and then pull your leg back (Fig. 3,4). You must do this as hard and as fast as you can (concentric test).
c. During the test the machine draws a graph of your strength on the computer.
d. Watch the computer and try to make the line go near the top of the computer by trying harder.
e. If you start feeling any pain in your legs or start feeling fatigue then stop straight away.
Once the measurements were done, the data about the child was put into the computer under a coded number. To protect the privacy of all test results, children are only identified by a subject number and name (Figures 3& 4).
Training procedure
I-Group (A): received traditional exercise program (Stretching exercises, Bobath approach, strengthening exercises, balance and gait training exercises). This program was done in approximately one hour, five times per week in 4 weeks [13].
II-Group (B): got both conventional exercise as well as lokomat gait training. Treadmill, weight support system, & two lightweight robotic actuators connected to the subject's legs composed the Lokomat system (Hocoma AG, Zurich, Switzerland) (Fig. 5). The treadmill's speed ranged from zero to almost three kilometers per hour. The treadmill was set at a constant 1.5 kilometers per hour during treatment. At the start of the treatment, the harness system supported about half of each subject's body weight. Following the subsequent walking sessions, the body weight support was decreased until the person could walk without their knees giving way or their toes dragging. The guidance force was kept between 70% and 100%, depending on how well the patient could handle it [14].
To get patients even more interested and motivated, computer game techniques could be used to create a virtual environment that encourages them to take an active role in their treatment.
Statistical analysis
Statistical analysis was performed using SPSS software for Windows, version 21.0 (Chicago, IL,United States). For both groups, descriptive statistics were made before and after 1 month. Shapiro-Wilk's test was used to check the normal distribution of data. Repeated measures multivariate analyses of variance, a two-way mixed model with the time within-subject factor, were utilized to determine any differences between the mean change scores of each group regarding Peak torque values of knee flexors and extensors (isokinetic measurements) using Biodex isokinetic dynamometer and The ability to walk using walking index for spinal cord injury version II (WISCI-II). The F value was used based on Wilks' lambda, and when the Multivariate Analysis of Variance (MANOVA) demonstrated a substantial effect (P<0.05), a follow-up univariate analysis of variance (ANOVA), a group-by-time two-way mixed model ANOVA with time as the repeated factor, was performed at P=0.01 to protect against the possibility of the type I error.
Result
This study is concerned in determining the effectiveness of lokomat gait training for improvement in ambulatory as well as lowering of disability level in patients having SCI. Clinical, functional and laboratory assessment data were collected from the CG who received regular physiotherapy and the SG who received the lokomat gait training along with traditional exercise treatment program given to the control group.
There was no substantial difference between groups in age, height and weight (P > 0.05) as illustrated in table 1. There was no substantial difference between both groups in gender distribution as the Chi-squared value was 0.53 (P > 0.05) (Table 1).
Characteristics |
Control group X ¯± SD | Study group X ¯± SD | p-value |
|---|---|---|---|
| Age (year) | 10.7 ± 3.4 | 10.4 ± 3.5 | 0.36 NS |
| Height (cm) | 138.3 ± 18 | 139.8 ± 16 | 0.62 NS |
| Weight (kg) | 45.3 ± 21 | 46.8 ± 22 | 0.73 NS |
| X ¯: Mean; SD: Standard deviation; P-value: Level of significance; NS: non- substantial |
|||
Muscular strength and gait abilities at entry and the end of the treatment 1. Peak torque values of knee flexors and extensors (isokinetic measurements).
Regarding right knee joint in the control group, there is substantial change between before and after treatment in the values of Knee flexors at 60 deg/sec, Knee extensors at 60 deg/sec, Knee flexors at 120deg/sec, & Knee extensors at 120 deg/sec (Table 2).
| Affected side | Peak torque values at(60 and 120 deg\sec) |
before X±SD | after X±SD | t value | P value | Significance |
| Right knee | Knee flexors at 60 deg/sec | 24.01±7.93 | 26.23±8.59 | -2.65 | 0.016 | S |
| Knee extensors at 60 deg/sec | 33.55±8.62 | 35.95±8.08 | -2.74 | 0.013 | S | |
| Knee flexors at 120deg/sec | 19.66±7.57 | 21.52±7.45 | -2.70 | 0.014 | S | |
| Knee extensors at 120 deg/sec | 29.69±8.09 | 31.57±8.23 | -2.49 | 0.022 | S | |
| X: mean; SD: Standard deviation; t value: paired t value; P value: Probability value; S: Substantial | ||||||
Regarding left knee joint in control group, there is substantial change between before and after treatment in the values of Knee flexors at 60 deg/sec, Knee extensors at 60 deg/sec, Knee flexors at 120deg/sec, & Knee extensors at 120 deg/sec (Table 3).
| Affected side | Peak torque values at(60 and 120 deg\sec) |
before X±SD | after X±SD | t value | P value | Significance |
|---|---|---|---|---|---|---|
| Left knee | Knee flexors at 60 deg/sec | 23.92±8.37 | 25.87±8.73 | -2.41 | 0.026 | S |
| Knee extensors at 60 deg/sec | 33.61±8.11 | 35.66±9.04 | -2.43 | 0.025 | S | |
| Knee flexors at 120deg/sec | 19.46±7.87 | 21.66±8.32 | -2.81 | 0.011 | S | |
| Knee extensors at 120 deg/sec | 29.52±8.29 | 31.50±8.79 | -2.61 | 0.017 | S |
Statistical analyses for study group (SG) were studied before and after treatment. The post treatment results of peak torque values of knee flexors & extensors showed substantial improvement (P<0.05).
Regarding right knee joint in study group, there is substantial change between before and after treatment in the values of Knee flexors at 60 deg/sec, Knee extensors at 60 deg/sec, Knee flexors at 120deg/sec, & Knee extensors at 120 deg/sec (Table 4).
| Affected side | Peak torque values at(60 and 120 deg\sec) |
before X±SD | after X±SD | t value | P value | Significance |
|---|---|---|---|---|---|---|
| Right knee | Knee flexors at 60 deg/sec | 24.35±8.01 | 34.39±8.79 | -7.39 | 0.000 | S |
| Knee extensors at 60 deg/sec | 33.64±7.81 | 41.21±8.69 | -6.50 | 0.000 | S | |
| Knee flexors at 120deg/sec | 19.35±7.37 | 30.41±9.74 | -7.44 | 0.000 | S | |
| Knee extensors at 120 deg/sec | 29.64±7.99 | 37.85±8.67 | -7.09 | 0.000 | S |
Regarding left knee joint in study group, there is substantial change between before and after treatment in the values of Knee flexors at 60 deg/sec, Knee extensors at 60 deg/sec, Knee flexors at 120deg/sec, and Knee extensors at 120 deg/sec (Table 5).
| Affected side | Peak torque values at(60 and 120 deg\sec) |
before X±SD | after X±SD | t value | P value | Significance |
|---|---|---|---|---|---|---|
| Left knee | Knee flexors at 60 deg/sec | 24.03±8.04 | 45.92±7.55 | -10.4 | 0.000 | S |
| Knee extensors at 60 deg/sec | 33.91±7.91 | 41.35±8.47 | -7.18 | 0.000 | S | |
| Knee flexors at 120deg/sec | 19.56±7.37 | 27.74±7.85 | -8.07 | 0.000 | S | |
| Knee extensors at 120 deg/sec | 29.78±8.11 | 38.07±9.51 | -5.28 | 0.000 | S |
2. The ability to walk was evaluated according to the walking index for spinal cord injury version II (WISCI-II).
Patients in the RAGT group showed substantial greater gain (from 3 [interquartile range (IQR), 0-14] to 11 [IQR, 0-19]) compared to controls in the WISCI-II (from 4 [IQR, 0–16] to 9 [IQR, 0-20]).
Discussion
After an average of four weeks of treatment, a SCI patient with an AIS-D rating revealed substantial increase in muscular strength & functional recovery, with favorable findings shown in the RAGT group. WISCI-II, which supported walking reeducation with RAGT, resulted in a dramatic reduction in the need for assistance. This RAGT procedure was not done as a replacement for more traditional forms of treatment. RAGT provided treatment that was objective, repeated, and qualitatively equivalent. Unfortunately, the feedback could not be immediate. Thus, the addition of RAGT to traditional physiotherapy may provide added benefits above conventional physiotherapy alone.
Alcoben-das-Maestro et al. did a randomized controlled trials (RACT) study with subacute SCI patients who had an incomplete SCL within 3 to 6 months. They found that the RAGT groups improved substantially from baseline to follow-up in terms of WISCI-II as well as walk distance [8]
Our findings are consistent with those of recent studies by Sophie et al., who found that robotic-assisted gait training (lokomat) provides a chance to improve walking practice with mechanical assistance from robotic devices, instead of therapists, in cases where the child may not be capable of generating enough or correct motion with adequate repetitions to promote gait improvement [7]
Using robotic technology to aid in the rehabilitation of neurological patients has various advantages. Long-term repetition of the exercise will impact the neurological system (in consideration of neuroplasticity) in addition to lightening the weight, facilitating balance in orthostatism, as well as developing a quasi-normal gait [15].
Establishing dynamic training programmes is an advantage of utilizing medical robots. One of the robotic gait rehabilitation devices is the computer-controlled & electrically operated orthosis Lokomat, which establishes an appropriate gait pattern and restores lost proprioception. [15].
Mehrholz et al. evaluated RCTs regarding the effect of locomotor training on the improvement of walking following severe SCI. Several methods of locomotor training didn't vary in terms of safety and acceptability for the majority of trial participants, according to the findings presented in this research. The authors observed insufficient data from RCTs to support a particular locomotor training technique for the improvement of walking performance in SCI patients [16].
In individuals with SCI, robot-assisted gait training is associated with improvements. Nevertheless, when findings are compared to other walking rehabilitation techniques, including walking over-ground or using a treadmill either with or without BWS, robot-assisted gait training does not produce greater improvements than other training modalities [17,18]. Many individuals with SCI can keep or get back their ability to walk, however their endurance and speed of walking may be affected [19].
These findings corroborate those of Quinzanos et al., who found that training using a robotic orthosis improved gait pattern in patients with partial SCI. No clear benefits of training for 30 vs. 60 minutes have been found as of yet. [20]
These findings were in accordance those of Pajaro et al., who found that RAGT increased children's walking velocity and endurance. [21]. The neuromuscular anomalies caused by spasticity can be greatly diminished with RAGT. [22].
Westlake and Patten conducted systematic studies that looked at the impact of partial body weight supported treadmill training for individuals who have cerebral palsy, spinal cord injuries, and traumatic brain injuries. A number of studies have shown that patients of various backgrounds who received robotassisted gait training experienced substantial increases in their locomotor capacity.[23]
Physiotherapists use traditional physical therapy including stretching, strengthening, as well as manual-assisted gait training, but the use of locomotor robotic devices improves their efficiency and effectiveness [24].The RAGT helps spinal cord injury patients keep their lifestyles healthy & raise their physical activity levels by normalizing muscle tone, regaining functional walking, and increasing lower extremity function. [25,26]
It has been reported that patients with subacute stroke or spinal cord injury benefit from RAGT, and that this training is more successful at promoting functional motions when applied for a longer duration and at a higher intensity, when used in conjunction with a general rehabilitation program. Nevertheless, there is not enough data to determine the most effective treatment strategy. [27, 28].
In addition, there is not enough evidence to suggest that RAGT improves gait speed, gait distances, lower extremity motor scores, spasticity level, or functional independence in individuals with SCI. [29].
Limitations
Our research had numerous limitations. The patients in each group were rather low, and their causes were various. Only short-term effects were assessed. No assessment of long-term follow-up was performed. Our findings indicated that RAGT may be a beneficial adjunct to gait training for SCI patients. Unfortunately, research did not provide sufficient evidence to assert that this type of instruction was superior to traditional technique. Even now, this study adds to the large amount of information needed to find the right candidate, the best time, also the best protocol to make RAGT work best for SCI patients.
Conclusion
It is possible that ambulatory function can be improved by RAGT when paired with traditional physiotherapy. In children with incomplete spinal cord injuries, RAGT can be a useful adjunct to other rehabilitative methods.
Competing interests:
We did not receive any financial support from any institution or company, it is our project, and we insured all expenses. No competing interests
Author contribution:
We are seven authors for this work, and we did all requirements to accomplish this work, there is no other researchers participate in this work.
Conflict of interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article
References
Nas, K.; Yazmalar, L.; ̧Sah, V.; Aydın, A.; Öne ̧s, K. Rehabilitation of spinal cord injuries. World J. Orthop.2015,6, 8–16.
Shin JC, Kim DH, Yu SJ, Yang HE, Yoon SY. Epidemio-logic change of patients with spinal cord injury. Ann Rehabil Med 2013;37:50-6.
Masterson k. Anew spinal cord injury treatment is getting patients back on their feet 2018.
Burns SP, Golding DG, Rolle WA Jr, Graziani V, Ditun-no JF Jr. Recovery of ambulation in motor-incomplete tetraplegia. Arch Phys Med Rehabil 1997;78:1169-72.
Van Middendorp JJ, Hosman AJ, Pouw MH; EM-SCI Study Group, Van de Meent H. ASIA impairment scale conversion in traumatic SCI: is it related with the abil-ity to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord 2009;47:555-60.
Dietz V, Colombo G, Jensen L, Baumgartner L. Loco-motor capacity of spinal cord in paraplegic patients. Ann Neurol 1995;37:574-82.
Sophie L, Remo R and Susan H. The effectiveness of robotic-assisted gait training for pediatric gait disorders: systematic review J. of neuro engineering and rehabilitation 2017; 14:1.
Alcobendas-Maestro M, Esclarin-Ruz A , Casado-L opez RM, Munoz-G onzalez A , Perez-Mateos G, Gonzalez-Valdizan E, et al. Lokomat robotic-assisted versus overground training within 3 to 6 months of incomplete spinal cord lesion: randomized controlled trial. Neurorehabil Neural Repair 2012;26:1058-63.
Picelli, A.; Melotti, C.; Origano, F.; Neri, R.; Waldner, A.; Smania, N. Robot-assisted gait training versus equal intensity treadmilltraining in patients with mild to moderate Parkinson’s disease: A randomized controlled trial.Park. Relat. Disord.2013,19,605–610.
VanNunen MPM,Gerrits KHL,deHaan A,Janssen TWJ.Exercise intensity of robot-assisted walking versus overground walking in nonambulatory stroke patients. JRehabil Res Dev 2012;49: 1537–46.
Riener R, Lunenburger L, Maier C et al. Locomotor training in subjects with sensorimotor deficits: An overview of the robotic gait orthosis lokomat. J healthcare engineering 2010; Vol 1. NO .2 PP 197-216.
Wilk K. (1990): Muscle strength testing: Instrumented and no instrumented systems. New York, Chruchill Livingstone, pp. 60-63, 123-150.
Bobath B. Adult hemiplegia: Evaluation and treatment. Oxford, Butterworth-Heinemann 1990; 3rd edition, 134-187.
Husemann B, Müller F, Krewer C et al. Effects of locomotion training with assistance of robot-driven gait orthosis in hemiparetic patients after stroke.Stroke 2007;38:349-54.
Domingo, A.; Lam, T. Reliability and validity of using the Lokomat to assess lower limb joint position sense in people withincomplete spinal cord injury.J. Neuroeng. Rehabil.2014,11, 167.
Mehrholz J, Kugler J, Pohl M. Locomotor training for walking 33. after spinal cord injury. Spine 2008; 33: E768–E777.
Field-Fote E, Lindley S, Sherman A. Locomotor training approaches for individuals with spinal cord injury: a preliminary report of walking-related outcomes. J Neuro Phys Ther 2005; 29: 127–137.
Hornby TG, Campbell dd, Zemon dH, Kahn JH. Clinical and quantitative evaluation of robotic-assisted treadmill walking to retrain ambulation after spinal cord injury. Top Spinal Cord Inj Rehabil 2005; 11: 1–17
Kim, C.M.; Eng, J.J.; Whittaker, M.W. Level walking and ambulatory capacity in persons with incomplete spinal cord injury:Relationship with muscle strength.Spinal Cord2004,42, 156–162.
Quinzanos J, Apodaca LF, Aguirre AV, Quinzanos I, Perez sanapablo AL, Perez zavalar R. Effect of two different programs of robotic assisted gait training in individuals with chronic motor incomplete spinal cord injury. J Annals physical and rehabilitation medicine,2018; 61:242.
Pajaro M, Shetye R, Gallegos J et al. Robotic-Assisted Gait Training in Children with Cerebral Palsy in Clinical Practice. In: Pons J., Torricelli D., Pajaro M. Converging Clinical and Engineering Research on Neurorehabilitation. Biosystems & Biorobotics 2013; vol 1. Springer pp 29-33
Mirbagheri MM, Kindig M, Niu X, Varoqui D, Con-away P. Robotic-locomotor training as a tool to reduce neuromuscular abnormality in spinal cord injury: the application of system identification and advanced longitudinal modeling. IEEE Int Conf Rehabil Robot 2013:6650497.
Westlake K and Patten C. Pilot study of lokomat versus manual assisted treadmill training for locomotor recovery post –stroke. J Neuroeng Rehabil 2009; 6: 18.
Hwang S, Kim HR, Han ZA, Lee BS, Kim S et al. Improved gait speed after robot-assisted gait training in patients with motor incomplete spinal cord injury: a preliminary study. Annals of Rehabilitation Medicine 2017; 41 (1): 34-41. doi: 10.5535/arm.2017.41.1.34
Fang, C.Y.; Tsai, J.L.; Li, G.S.; Lien, A.S.Y.; Chang, Y.J. Effects of Robot-Assisted Gait Training in Individuals with Spinal CordInjury: A Meta-analysis.Biomed. Res. Int.2020, 2102785.
Nam, K.Y.; Kim, H.J.; Kwon, B.S.; Park, J.W.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking functionand activity in people with spinal cord injury: A systematic review.J. Neuroeng. Rehabil.2017,14, 24–36.
Bae, Y.H.; Kim, Y.H.; Shirley, S.M. Comparison of heart rate reserve-guided and ratings of perceived exertion-guided methods forhigh-intensity robot-assisted gait training in patients with chronic stroke: Focused on the motor function and gait ability.Top.Geriatr. Rehabil.2016,32, 119–126.
Bae, Y.H.; Lee, S.M.; Ko, M. Comparison of the effects on dynamic balance and aerobic capacity between objective and subjectivemethods of high-intensity robot-assisted gait training in chronic stroke patients: A randomized controlled trial.Top. Stroke Rehabil.2017,24, 309–313.
Nam KY, Kim HJ, Kwon BS, Park JW, Lee HJ et al. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: a systematic review. Journal of Neuroengineering and Rehabilitation 2017; 14 (1): 24. doi: 10.1186/s12984-017-0232-3.