Research Article - (2024) Volume 19, Issue 5
EVALUATION OF PATIENT-REPORTED OUTCOME AND SATISFACTION FOLLOWING PERCUTANEOUS CORONARY INTERVENTION: A SYSTEMATIC REVIEW
Muhannad A Almubarak1*, Sultan Ayed K Alanazi2, Nawaf Abdulaziz M Alzarea2, Waleed Abdullah A Alzarea2, Ahmed Hamoud E Alkhaldi2, Salem Ibrahim S Aljaddua2, Fahad Naif M Alruwaili2, Sayyaf Falah S Alruwaili2, Omar Mohammed A Alshaya2, Sultan Farhan O Alruwaili2, Norah Farhan O Aldaghmani2 and Yaser Abdulkareem J Aldheli2*Correspondence: Muhannad A Almubarak, Assistant Professor of internal medicine at Al-Jouf university &Consultant internal medicine and Adult cardiology & interventional cardiology in King , Saudi Arabia, Email:
Abstract
Background: A growing number of elderly patients with satisfactory periprocedural outcomes and long-term survival are undergoing percutaneous coronary intervention (PCI).
Objective: To systematically review patient satisfaction after PCI.
Methods: An extensive search of PubMed, Web of Science, Scopus, and Science Direct was performed to locate relevant material. Rayyan QRCI was used to select the eligible articles. Results: Our data includes seven articles with 4278 children, 3378 (78.9%) of whom were males. The reported follow-up duration ranged from 3 days to 36 months. Seven studies reported a high satisfaction level following PCI. It is reported that same-day discharge corresponds with more problems. Only one study included patients who reported moderate satisfaction levels according to the SAQ-Korean version.
Conclusion: This review found that there is a high patient-reported satisfaction among patients who underwent PCI. Larger prospective trials are needed to determine the long-term satisfaction and QOL following PCI.
Keywords
Percutaneous coronary intervention; Satisfaction; Quality of life; systematic review.
Introduction
Globally, cardiovascular disease is the primary cause of death [1]. The World Health Organization (2020) estimates that 17.9 million fatalities worldwide in 2017 were attributed to cardiovascular disease or 31% of all deaths. For the past 15 years, it has remained the primary cause of death worldwide [2]. According to projections made by the World Health Organization (2012), coronary heart disease and stroke will account for roughly 23.6 million deaths worldwide from cardiovascular disease by the year 2030 [3]. In underdeveloped nations with low to moderate incomes, cardiovascular disease accounts for more than 75% of fatalities [4].
A degenerative heart ailment linked to societal socioeconomic situations and lifestyle choices is coronary heart disease [5]. Atherosclerosis, a disorder that affects the form and function of the arteries, is brought on by an abnormal buildup of lipids, fatty materials, and fibrous tissue in the blood channel walls. The heart may not receive enough blood due to atherosclerosis, and the heart muscle cells might not contain any blood [6]. As a result, the patient will have ischemia in the heart muscles, which may result in chest pain and, in more extreme cases, irreversible damage to the heart cells [7]. PCI, a non-surgical procedure that dilates the coronary arteries, can improve ischemia regions and blood supply to the myocardium [7].
An invasive treatment known as PCI, or cardiac catheterization, involves inserting one or more catheters into the heart and certain blood vessels. 954,000 people in the US have had PCI operations, according to the American Heart Association's 2017 heart disease and stroke data [8]. In our opinion, QOL can play a significant role in determining how best to manage a patient, particularly when it comes to indications where there are gray areas. Quality of life (QOL) is a crucial consequence of any medical procedure, and for many, it is just as important as or even more important than extending life expectancy. Any treatment plan's main objective and advantage is unquestionably to improve QOL [9].
We aim to systematically review patient satisfaction after PCI.The existing literature may have limited scope, methodological variations, or focus on specific age groups. A systematic review is necessary to synthesize available evidence, identify knowledge gaps, and inform future research and clinical practice. There is a dearth of evidence on patient-reported satisfaction following cardiac interventions.
Methods
We conducted this systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [10] criteria. A computerized search was conducted on databases such as PubMed, Web of Science, SCOPUS, and Science Direct to discover English-language research. Relevant keywords were used in the search method in these scenarios: “percutaneous coronary intervention,” “PCI,” “Patient satisfaction,” and “Quality of life.”. Two reviewers separately searched through the search outcomes, chose relevant papers, collected data, and utilized the appropriate assessment procedures to establish how strong the included study was.
Eligibility Criteria:
Inclusion Criteria
- Study population: Patients underwent PCI.
- Study design: Cross-sectional, cohort, case-control, or randomized controlled trials (RCTs).
- Outcome measures: Evaluation of post-intervention QoL including satisfaction.
- Language: Studies in English.
Exclusion Criteria
- Case reports, case series, reviews, editorials, or commentaries.
- Studies published in languages other than English.
- with a critical methodological flaw that significantly compromises the validity of the results.
Data Extraction
Rayyan (QCRI) was utilized to check the search results and ensure accuracy [11]. The inclusion and exclusion criteria were employed to establish the relevance of the titles and abstracts. The study team thoroughly reviewed papers that met the inclusion criteria. Consensus was employed to resolve disputes. Key study data will be recorded using an established data extraction form, including titles, authors, publication year, study location, gender distribution, participant demographics, satisfaction assessment tool, follow-up duration, and main outcomes. To investigate the probability of bias, a neutral evaluation instrument was developed.
Data Synthesis Strategy
Summaries of the research outcomes and aspects were generated using information from relevant studies in order to provide a qualitative assessment. The optimum technique to ensure the use of the data from the included studies was determined upon after gathering the information for the systematic review was completed.
Risk of Bias Assessment
The study's quality was assessed using the critical assessment criteria for studies reporting prevalence data developed by the Joanna Briggs Institute (JBI) [9]. This tool contained nine questions. A one was provided for a favorable response, and a zero for a negative, ambiguous, or irrelevant response. The following scores will be classified as poor, moderate, or high quality: less than 4, between 5 and 7, and greater than 8. Researchers rated the quality of the studies separately, and disagreements were resolved through discussion.
Results
Systematic search outcomes
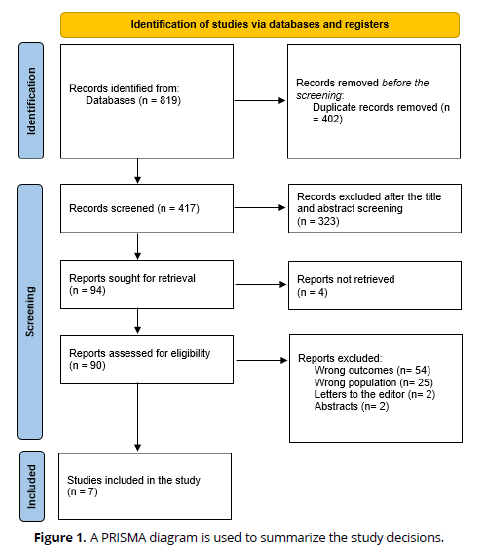
Following the removal of 819 duplicates, a systematic search yielded 402 study papers. After 417 studies' titles and abstracts were reviewed, 323 papers were rejected. Out of the 94 reports that needed to be obtained, just 4 articles were not found. 90 articles passed the full-text screening procedure; 54 were rejected owing to inaccurate study results, 25 were due to improper population type, 2 were editor's letters, and 2 were abstracts. Seven of the research publications included in this systematic review met the eligibility criteria. Figure 1 depicts an overview of the approach used to choose the research.
Sociodemographics of the comprised participants and studies
Table 1 displays the sociodemographic information from the research articles. Our data includes seven articles with 4278 children, 3378 (78.9%) of whom were males [10-19]. Two studies were cross-sectional [14, 19], two were prospective cohorts [13, 15], two were RCTs [17, 18], and one was a retrospective cohort [16]. One study was conducted in Pakistan [13], one in South Korea [14], one in the USA [15], one in Switzerland [16], one was multi-centered [17], one in Armenia [19], and one in the USA and Canada [18]. The earliest study was conducted in 2003 [17] and the latest in 2024 [13].
Clinical outcomes
| Study | Study design | Country | Participants | Mean age | Males (%) |
|---|---|---|---|---|---|
| Khan et al., 2024 [13] | Prospective cohort | Pakistan | 220 | 62 | 120 (54.5%) |
| Kim et al., 2019 [14] | Cross-sectional | South Korea | 124 | 61.7 ± 10.8 | 98 (79%) |
| Amin et al., 2018 [15] | Prospective cohort | USA | 230 | 62.4 ± 11.7 | 183 (79.6%) |
| Biasco et al., 2017 [16] | Retrospective cohort | Switzerland | 312 | 66.6 ± 10.8 | 205 (65.7%) |
| Zhang et al., 2003 [17] | Prospective RCT | Multi-centered | 988 | 61.4 | 780 (79%) |
| Sedlis et al., 2013 [18] | RCT | USA and Canada | 2029 | 68 ± 9 | 1754 (86.4%) |
| Aghabekyan et al., 2012 [19] | Cross-sectional | Armenia | 375 | 57.5 ± 9.8 | 238 (87.8) |
Table (2) presents the clinical findings of our included participants. The reported follow-up duration ranged from 3 days [16] to 36 months [18]. Patient satisfaction assessment was carried out using multiple tools including the Seattle Angina Questionnaire (SAQ) [14, 17, 18], post-discharge telephone follow-up questionnaire [15, 16], Cardiac Patient Satisfaction Questionnaire (CPSQ) [13], and the Patient Satisfaction Questionnaire (PSQ-18) [19]. Seven studies reported a high satisfaction level following PCI [13, 15-19]. It is reported that same-day discharge corresponds with more problems [13, 15]. Only one study included patients who reported moderate satisfaction levels according to the SAQ-Korean version [14].
| Study ID | Satisfaction assessment tool | Follow-up (months) | Main outcomes | JBI |
|---|---|---|---|---|
| Khan et al., 2024 [13] | CPSQ | 1 | Same-day discharge corresponds with more problems even when patient satisfaction is higher, indicating a need for caution. | Moderate |
| Kim et al., 2019 [14] | SAQ-Korean version | 1 | Individuals with cardiovascular disease who had a PCI had a moderate overall health-related QoL, physical limits, treatment satisfaction, and disease perspective. | High |
| Amin et al., 2018 [15] | A post-discharge telephone follow-up questionnaire | 1 | Nearly all of the patients who were discharged that same day expressed very high levels of patient satisfaction. | Moderate |
| Biasco et al., 2017 [16] | A post-discharge telephone follow-up questionnaire | 3 (days) | In 97% of the cases, patients claimed total satisfaction. | NA* |
| Zhang et al., 2003 [17] | SAQ | 12 | Both the PCI and CAP therapy groups reported high levels of treatment satisfaction. | NA* |
| Sedlis et al., 2013 [18] | SAQ | 36 | At the beginning of both the PCI and medical therapy groups, the treatment satisfaction levels were high and did not show any discernible changes. | Moderate |
| Aghabekyan et al., 2012 [19] | PSQ-8 | 12 | Nork Marash Medical Center PCI patients gave very high ratings to every one of these categories of satisfaction. | Moderate |
CPSQ=Cardiac Patient Satisfaction Questionnaire, SAQ=the Seattle Angina Questionnaire, PSQ-18=the Patient Satisfaction Questionnaire.
Discussion
According to our knowledge, this is the first systematic review to comprehensively investigate patient-reported satisfaction after undergoing PCI. This review was limited by its qualitative evaluation, however, our search comprised multiple major databases.
Seven studies in this review reported a high satisfaction level following PCI [13, 15-19]. It is reported that same-day discharge corresponds with more problems [13, 15]. Only one study included patients who reported moderate satisfaction levels according to the SAQ-Korean version [14]. Three studies used the SAQ tool, compared to other health status measures, such as the SF-36, the SAQ is thought to be a superior assessor of clinical health status due to its higher sensitivity and easier interpretability. The physical limitation score, angina frequency score, treatment satisfaction score, and angina stability score are the five dimensions that make up this assessment. Soo Hoo et al. reported that following PCI, everyone exhibited improvements in their level of physical function, frequency of angina attacks, disease burden, and satisfaction with their therapy. However, more investigation is required to assess the wider physical and psychological requirements of elderly patients during the PCI recovery process. Of particular interest is the effect that aging and frailty have on health-related QO) when fast-paced PCI pathways, like pre-hospital STEMI diagnosis and early field triage to PCI, are in place [20].
Shan et al. also found that elderly patients' health-related QOL can improve following PCI for a minimum of a year in a number of health areas, and it is similar to that of younger patients having PCI and the age-matched general population [21].
Our findings are highly relevant to nursing practice. The current treatment of PCI patients frequently does not address all of these components, and the health-related QOL score indicates a holistic approach to the physiological and psychological aspects of rehabilitation. Seldom is the health-related QOL evaluated or discussed with PCI patients. Other characteristics that have been found to affect health-related QOL recently include gender, frailty, and poor health status; however, these factors are not commonly examined using PCI [22, 23]. In spite of its possible influence on mortality, morbidity, HRQOL results, and major cardiac incidents like restenosis after PCI, there is little information available on cardiac rehabilitation attendance patterns following emergency PCI for older adults [24, 25]. These broader aspects of care delivery are also still poorly studied. Future studies should additionally distinguish between the outcomes of primary and elective PCI.
Limitations
It is important to take into account the many restrictions that apply to our systematic study. Some relevant research might have been left out because of the single database and English language constraint. The diverse assessment tools may be also a source of bias in this review. Only 8 studies met our inclusion criteria with a small sample size.
Conclusion
This review found that there is a high patient-reported satisfaction among patients who underwent PCI. Larger prospective trials are needed to determine the long-term satisfaction and QOL following PCI.
References
World Health Organization. (April, 2020). Retrieved July 15, 2024 from https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1
World Health Organization. (December, 2018). Retrieved July 15, 2024 from https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
World Health Organization. (March, 2012). Retrieved July 15, 2024 from https://www.who.int/cardiovascular_diseases/about_cvd/en/
Depkes.go.id. (November, 2018). Retrieved July 15, 2024 from https://www.kemkes.go.id/article/view/18111200002/rs-jantung-harapan-kita-pengampurujukan-kardiovaskular.html
Iskandar I, Hadi A, Alfridsyah A. Faktor risiko terjadinya penyakit jantung koroner pada pasien Rumah Sakit Umum Meuraxa Banda Aceh. AcTion: Aceh Nutrition Journal. 2017 May 15;2(1):32-42.
Smeltzer SC, Bare BG, Hinkle JL, Cheever KH, Townsend MC, Gould B. Brunner and Suddarth’s textbook of medicalsurgical nursing 10th edition. Philadelphia: Lipincott Williams & Wilkins; 2008.
Tahhan AI, Al-Saigh TH. Effectiveness of an Educational Program on Nurses' Knowledge Regarding Post Thyroidectomy Nursing Management in Nineveh Governorate Hospitals.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, De Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. circulation. 2017 Mar 7;135(10):e146-603.
Noyez L, de Jager MJ, Markou AL. Quality of life after cardiac surgery: underresearched research. Interactive cardiovascular and thoracic surgery. 2011 Nov 1;13(5):511-5.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International journal of surgery. 2021 Apr 1;88:105906.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Systematic reviews. 2016 Dec;5:1-0.
Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, Lockwood C, Stephenson M, Moola S, Lizarondo L, McArthur A. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). JBI evidence implementation. 2019 Mar 1;17(1):36-43.
Khan FR, Nawaz T, Amin M, Sajjad W, Ali H, Hussain S. The Impact of Age, Comorbidities, and Discharge Timing on Clinical Outcomes Following Elective Percutaneous Coronary Intervention. Cureus. 2024 Feb;16(2).
Kim HS, Kim HK, Kang KO, Kim YS. Determinants of health‐related quality of life among outpatients with acute coronary artery disease after percutaneous coronary intervention. Japan Journal of Nursing Science. 2019 Jan;16(1):3-16.
Amin AP, Crimmins‐Reda P, Miller S, Rahn B, Caruso M, Pierce A, Dennis B, Pendegraft M, Sorensen K, Kurz HI, Lasala JM. Novel patient‐centered approach to facilitate same‐day discharge in patients undergoing elective percutaneous coronary intervention. Journal of the American Heart Association. 2018 Feb 15;7(4):e005733.
Biasco L, Pedrazzini GB, Araco M, Petracca F, Del Monte D, Sürder D, Bomio F, Berto MB, Montrasio G, Del Bufalo A, Pasotti E. Evaluation of a protocol for same-day discharge after radial lounge monitoring in a southern Swiss referral percutaneous coronary intervention centre. Journal of Cardiovascular Medicine. 2017 Aug 1;18(8):590-5.
Zhang Z, Mahoney EM, Stables RH, Booth J, Nugara F, Spertus JA, Weintraub WS. Disease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery: one-year results from the Stent or Surgery trial. Circulation. 2003 Oct 7;108(14):1694-700.
Sedlis SP, Jurkovitz CT, Hartigan PM, Kolm P, Goldfarb DS, Lorin JD, Dada M, Maron DJ, Spertus JA, Mancini GJ, Teo KK. Health status and quality of life in patients with stable coronary artery disease and chronic kidney disease treated with optimal medical therapy or percutaneous coronary intervention (post hoc findings from the COURAGE trial). The American journal of cardiology. 2013 Dec 1;112(11):1703-8.
Aghabekyan S, Thompson ME, Abrahamyan L. Medication noncompliance and patient satisfaction following percutaneous coronary intervention. Journal of Interventional Cardiology. 2012 Oct;25(5):469-75.
Soo Hoo SY, Gallagher R, Elliott D. Systematic review of health‐related quality of life in older people following percutaneous coronary intervention. Nursing & health sciences. 2014 Dec;16(4):415-27.
Shan L, Saxena A, McMahon R. A systematic review on the quality of life benefits after percutaneous coronary intervention in the elderly. Cardiology. 2014 Aug 5;129(1):46-54.
Schenkeveld L, Pedersen F, Van Nierop JW et al. Health-related quality of life and long-term mortality in patients treated with percutaneous coronary intervention. Am. Heart J. 2010; 159: 471–476.
Singh M, Rihal C, Lennon R, Spertus JA, Sreekumaran Nair K, Roger V. Influence of frailty and health status on outcomes in patients with coronary disease undergoing percutaneous revascularization. Circ. Cardiovasc. Qual. Outcomes 2011; 4: 496–502.
Jamieson M, Wilcox S, Webster W, Blackhurst D, Valois R, Durstine L. Factors influencing health-related quality of life in cardiac rehabilitation patients. Prog. Cardiovasc. Nurs. 2002; 17: 124–131.
Gharacholou S, Roger VL, Lennon RJ, Sloan JA, Spertus JA, Singh M. Comparison of frail patients versus nonfrail patients ≥ 65 years undergoing percutaneous coronary intervention. Am. J. Cardiol. 2012; 109: 1569–1575.