Research Article - (2024) Volume 19, Issue 3
FUNCTIONAL OUTCOME AND RECURRENCE RATE OF ARTHROSCOPIC BANKART REPAIR IN OMANI PATIENTS
Amro Magdy Elemam1*, Sulaiman Nasser Al Hamimi2*, Muhannad Mohamed Al Hunaini1 and Ahmed Al Mandhari1*Correspondence: Amro Magdy Elemam, Ministry of health-Oman, Khoula hospital, Egypt, Email: Sulaiman Nasser Al Hamimi, Ministry of health-Oman, Nizwa hospital, Egypt, Email:
Abstract
Background: Traumatic anterior glenohumeral dislocation is one of the most common traumatic joint disorders in young and active individuals.
Aim: To study the functional outcome and post-operative recurrence rate of recurrent shoulder instability operated by arthroscopic anterior stabilization in Omani patients.
Study design: retrospective case series study.
Methods: From 2015 to 2018, 69 patients underwent arthroscopic bankart repair at Khoula hospital, with a median follow-up of 20.49 months. Of these, 41 visited the clinic for scoring, while 29 were surveyed over the phone for recurrence using three scores: Oxford shoulder score, constant score, and Carter Rowe score.
Results: Among the 70 patients 6 (8,5%) patients had recurrence of dislocation. With oxford shoulder score, 78% (32 patients) had satisfactory results and 17,1% (7patients) had mild to moderate and 7% (2 patients) had moderate to severe. At constant score, 36,6% (15 patients) of the patients had excellent results, 29,3% (12 patients) had good results 12,2% (5) patients had fair results and 22% (9 patients) had poor results. Patients not receiving post-operative physiotherapy had worse Rowe scores and Oxford functional outcomes. Military patients had worse results than labor workers, and labor workers performed worse than office workers.
Conclusion: Anterior shoulder instability is challenging for young patients with high demands. External rotation deficit affects functional outcome and patient satisfaction. Results are comparable to published literature but recommend larger studies.
Keywords
Functional outcome, Recurrence rate, Arthroscopic bankart repair
Introduction
Traumatic anterior glenohumeral dislocation is one of the most common traumatic joint disorders in young and active individuals. The reported yearly incidence rate in USA is about 24 per 100 000 person where 71,8% of them are males. About 46,8% of the dislocations were in patients between fifteen and twenty-nine years of age (1).
This injury commonly results in recurrent glenohumeral instability (2).Bankart was the first author to recognize the pathognomonic lesion of anterior-inferior capsulolabral disruption associated with anterior shoulder dislocations (3). It is well accepted that patients with recurrent instability are in need for surgical intervention and many surgical techniques were described (4). Anterior repair of the capsule and glenoid labrum was first described by Perthes in 1906 reporting excellent functional outcome (5). Consequently, repair of the anterior capsulolabral disruption has become the standard treatment for this pathology as it addresses the pathology (6,7). The aim of this surgery is to restore shoulder stability, improve shoulder function as well as relieve discomfort (8).
Surgical treatment was only performed with open procedures to repair the lesion with or without a capsular shift (9). Along with improvement of the surgical arthroscopic techniques and implants for repair of the Bankart lesion, arthroscopic repair of bankart lesion is becoming more common along with open surgeries (10).
As this procedure results are not studied before in our population, the purpose of this retrospective case series study is to study the functional outcome and post-operative recurrence rate of recurrent shoulder instability operated by arthroscopic anterior stabilization in Omani patients. Arthroscopic repair has been started in Khoula hospital-a tertiary referral hospital- for period of five years.
Patients and methods
Ethical approval was taken from Khoula hospital ethical committee. All patients were consented for involvement in the research.
Seventy-nine patients were operated for arthroscopic bankart repair during the period from January 2015 till February 2018 at Khoula hospital, Oman, Muscat. Three were females and the rest were males (77 patients). All operations were done by two independent surgeons.
Exclusion criteria included all patients with revision surgery, patients under 18 years of age or more than 45 years of age and patient with other injuries other than bankart lesion, eg, rotator cuff tear and associated fractures.
seventy patients were contacted through a phone call and recurrence of dislocation were explored and were invited for outpatient clinic for further clinical examination.
Of the 70 patients, total 41 patients were able to come to the clinic. the participant was asked to fill three validated scoring system questionnaires followed by clinical examination measuring the range of movement, signs of instability and strength.
Three scores were used. First oxford shoulder score, which is subjective score to measure the patient daily activity, this score is filled by the patient himself.
Second score was constant score, which is a validated objective score to measure the range of movement and power of the affected limb.
Third score was the Carter Rowe score, and it is mainly measuring the instability, range of movement pain and ability to do work and sports.
In regards to physiotherapy, patients were categorized into three groups, compliant to physiotherapy patients those who attended more than 80% of the sessions, partially compliant for who attended between 50 % to 80% of the sessions and non-compliant patients who attended less that 50% of the sessions. The data were taken from the patient themselves.
We measured the external rotation and measured it to the contralateral side by using goniometer.
All the questionnaires were obtained by one doctor and filled by the patients.
All patients were seen and examined by one doctor.
Preparation for surgery
All patients were assessed and reviewed initially in the clinic for clinical examination.
The anterior posterior and lateral axillary shoulder x-rays were taken.
Bankart lesion was confirmed by MRI scan in all patients.
All patients were seen by anesthetist for evaluation for anesthesia. Patients were sent for 3 months course of pre-operative physiotherapy and rehabilitation.
Surgical technique
All patients were put is beach chair position and shoulder table. Initially the posterior portal is made after locating the posteriolateral border of acromion then about 2 cm inferior and 2 cm medial and entry made and the scope is inserted. After that, with assistance of the arthroscopy two anterior portals were made and 4,5mm cannula is inserted at one of the anterior portals. The anterio-inferior glenolabral margin is refreshed with rasp and capsular shift is done and stabilized with the first bioabsorbable 3 mm biocomposite suturetak anchor. Between 2 and 4 anchors were used is all cases.
After surgery
All patients were sent for physiotherapy and rehabilitation from the first post-operative day.
The instructions were given with plan of exercise below shoulder movement for the first three weeks then start progressing to full range of movement. The physiotherapy program is carried over 12 weeks. For the first six weeks patient is seen twice per week and for the next 6 weeks once per week.
Strengthening and scapula control exercises were started after six weeks from surgery. Patients are allowed to go for full activity after 6 months from surgery.
Follow up
For the patients with clinical follow up, the median follow up was 20, 49 months with minimum follow up of 6 months and maximum follow up of 42 months.
Statistical reports
The data were entered and analyzed by SPSS program. The level of significance was set at P <.1. For the assessment between pairs of qualitative variables, we use independence tests like the chi-square test. On the other hand, the ANOVA is used to compare a quantitative variable that has normal distribution with a categorical variable, we used. In this study, we used the Tukey test for a multiple comparisons test that has a difference in at least one average
Results
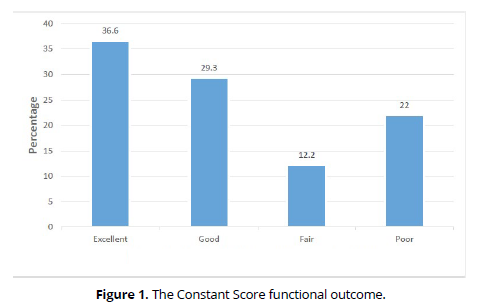
Among the 41 patients, the mean age of the patients was 29 years with minimum age was 18 years and maximum age was 45 years. With oxford shoulder score, 78 percent (32 patients) had satisfactory results and 17,1 percent (7patients) had mild to moderate and 7 percent (2 patients) had moderate to severe (Figure 1).
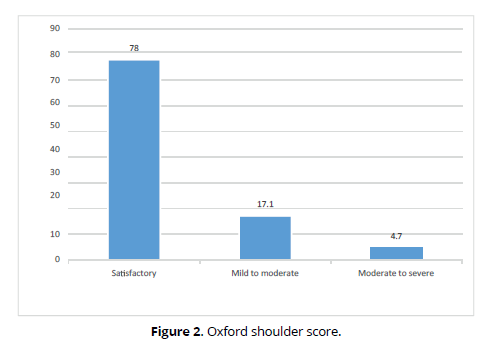
At constant score, 36,6% (15 patients) of the patients had excellent results, 29,3% (12 patients) had good results 12,2 % (5) patients had fair results and 22% (9 patients) had poor results (Figure 2).
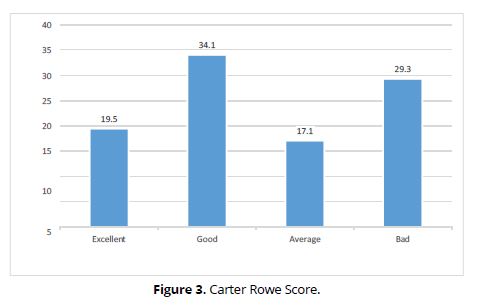
With Carter Rowe score, 19,5% (8 patients) had excellent results, 34,1% (14 patients) had good results, 17.1 (7patients) had average results and 29,3% (12 patients) had bad results (Figure 3).
Among the 70 patients were contacted, 6 (8,5%) patients had recurrence of dislocation. Four of the recurrences were traumatic and two were non traumatic. When compared to the normal side, the mean loss of external rotation on the affected side was 17.56 degrees. With regards to compliance to postoperative physiotherapy, 73,2% of the patients were compliant to physiotherapy, 19,5% were partially complaints and 7,3% were non-compliant to post-operative physiotherapy. And there was significant relationship between the compliance to physiotherapy and Rowe score with P values of 0,028. When looking to the relationship between the degree of loss of external rotation and the functional outcome, it was showing significant relationship between the degree of loss and the oxford functional outcome with P value of 0.01, as well seen between Carter Rowe score and loss of external rotation with P values of 0.029.
Patient who are working in military has worse oxford results compared to labour and office workers, and office workers performed better than labour workers with P value of 0.043 (Table 1).
| Type of work | Oxford score | ||
|---|---|---|---|
| Moderate to severe (20- 29) |
Mild to moderate (30- 39) |
Satisfactory (40-48) | |
| Office | 5.0% | 5.0% | 90.0% |
| Labour | 0.0% | 10.0% | 90.0% |
| Military | 9.1% | 45.5% | 45.5% |
But there was no significant relationship between type of work and constant shoulder score and Carter Rowe score. With regards to return to the pre injury sport level of activity, 41,5% were able to return their level of activity and 58,5 didn’t. There was significant relationship between the number of dislocations and functional outcome with all three scores. Highest is with carter rowe score with results of 0.056, then constant score of 0.093, and finally oxford score of 0.484.
Discussion
The reported recurrence rate of anterior shoulder dislocation after arthroscopic bankart repair varies between 7.5-35 %11, 12,13,14,15. Whereas our recorded recurrence rate is 8,5 which lies at this range. We have noticed highly variable results which is mainly due to the differences is the duration of follow-up and the definition of recurrence. For instance, some authors consider subluxation as recurrence which gives higher recurrence rate in their papers12, 16. In some studies even apprehension was defined as recurrence or failure of surgery17 .In our study we made our questionnaires with in the clinic which helped to emphasize the point if the patient feels subjective dislocation rather than apprehension as we didn’t consider it as failure.
Kim et al did a prospective study of 167 patients with mean follow up of forty-four months with carter Rowe score and reported 78% of his cases had excellent results and 17 % had good results18. Gartsman et al, studied 53 patients and reported mean of 91.8 points with the system of Constant score and mean of 91.9 points with Rowe score19.
With 13 years of follow up, Mohamed et al studied a case series of 180 patients post arthroscopic repair and resulted Rowe median of 90.0 and median constant score of 9413.
In our study, we found that the mean loss of external rotation was 17,5 degrees. Mohamed et al studied the deficit of external rotation and found it to be 13,4 degrees13. In another study, Hans et al studied the loss of external rotation on patients post open bankart repair and the mean was 12 degrees. At the same study, he found significant relationship between patient satisfaction at Rowe score and the amount of loss of external rotation20. In our study, this was evident with oxford shoulder score and Rowe score. There are very limited number of studies relating patient satisfaction and loss of external rotation in bankart repair which needs to emphasized more with larger number studies.
There are different factors affect the outcome of bankart repair reported in previous studies. Surgical implants and techniques differed between surgeons which consequently gives different outcomes19,21 . In his systemic review, Leroux et al found using 3 or more suture anchores improved recurrence rate to 8.7%22. All our patients had minimum of 3 suture anchors and we got similar recurrence rate.
In our study we found the higher number of dislocations associated with worse outcome in all the three scores. Gerometta A found patients with more numbers of dislocations before surgery return to sports later than patients with less number of dislocations19. This was explained by the irreversible progressive damage caused by successive dislocations of the joint23. It’s well understood currently that humeral bone loss increases the risk of failure in operated patients and this needs to be addressed surgically commonly with Remplissage procedure24, 25 .
In our study we found significant association between compliance to physiotherapy and functional outcome at carter row score. The importance of physiotherapy post arthroscopic bankart repair was emphasized in previous papers, but on the other hand there is very limited evidence supporting this aspect and the guidelines are very variable26, 27. Kim et al did and prospective study Comparing delayed rehabilitation after immobilization for 3 weeks and another group of patients starting range of movement exercises at immediate post operative day. With mean follow up of 31 months, the study showed patients with immediate rehabilitation has less pain and return to normal activity at earlier stage28. The importance of compliance to physiotherapy needs to be more investigated in further studies with larger number patients.
Only 41.5 % of our patients feel that they are able to return to the pre injury level of sports activity. Based on an objective criterion, Wilson et all found that 88.4% of their patients didn’t reach the appropriate level of function and strength of the affected shoulder after 6 months from the surgery29. In a systemic review study, it was found that only 66% of patients after arthroscopic bankart repair return to the pre injury level of sports30.
Conclusion
Anterior shoulder instability remains as challenge as most of the patients are young with high demands. Degree of external rotation deficit has role in patient satisfaction. Our group of patient’s results are comparable to the published literature. Post operative physiotherapy is crucial and should be emphasized as a part of the post operative treatment. However, we recommend further study with larger number of patients and follow up period will give more accurate representation.
Limitations
The number of patients involved in the study is limited. Larger number of patients with longer period of follow up will give more solid evidence. Furthermore, none of our treated patients were professional players, and such group patients is highly affected with this sort of injury and the outcome needs to be investigated.
Disclosure
The authors declarad no conflicts of interest and there are no financial conflicts of interest to disclose.
References
Zacchilli M, Owens B. Epidemiology of Shoulder Dislocations Presenting to Emergency Departments in the United States. The Journal of Bone and Joint Surgery-American Volume. 2010;92(3):542-549.
Matsen F, Zuckerman J. Anterior Glenohumeral Instability. Clinics in Sports Medicine. 1983;2(2):319-338.
Bankart A. The pathology and treatment of recurrent dislocation of the shoulder-joint. British Journal of Surgery. 1938;26(101):23-29.
Owens B, Dickens J, Kilcoyne K, Rue J. Management of Mid-season Traumatic Anterior Shoulder Instability in Athletes. Journal of the American Academy of Orthopaedic Surgeons. 2012;20(8):518-526.
Perthes. Über Operationen bei habitueller Schulterluxation. Deutsche Zeitschrift für Chirurgie. 1906;85(1):199-227.
Ide J, Maeda S, Takagi K. Arthroscopic Bankart Repair Using Suture Anchors in Athletes. The American Journal of Sports Medicine. 2004;32(8):1899-1905.
Mazzocca A, Brown F, Carreira D, Hayden J, Romeo A. Arthroscopic Anterior Shoulder Stabilization of Collision and Contact Athletes. The American Journal of Sports Medicine. 2005;33(1):52-60.
Rockwood C, Matsen F, Wirth M, Lippitt S, Fehringer E, Sperling J. Rockwood and Matsen's the shoulder.
Guanche C, Quick D, Sodergren K, Buss D. Arthroscopic Versus Open Reconstruction of the Shoulder in Patients with Isolated Bankart Lesions. The American Journal of Sports Medicine. 1996;24(2):144-148.
Netto N, Tamaoki M, Lenza M, Santos J, Matsumoto M, Faloppa F et al. Treatment of Bankart Lesions in Traumatic Anterior Instability of the Shoulder: A Randomized Controlled Trial Comparing Arthroscopy and Open Techniques. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2012;28(7):900-908.
Vermeulen A, Landman E, Veen E, Nienhuis S, Koorevaar C. Long-term clinical outcome of arthroscopic Bankart repair with suture anchors. Journal of Shoulder and Elbow Surgery. 2019;28(5):e137-e143.
van der Linde J, van Kampen D, Terwee C, Dijksman L, KleinJan G, Willems W. Long-term Results After Arthroscopic Shoulder Stabilization Using Suture Anchors. The American Journal of Sports Medicine. 2011;39(11):2396-2403.
Aboalata M, Plath J, Seppel G, Juretzko J, Vogt S, Imhoff A. Results of Arthroscopic Bankart Repair for Anterior-Inferior Shoulder Instability at 13-Year Follow-up. The American Journal of Sports Medicine. 2016;45(4):782-787.
GARTSMAN G, RODDEY T, HAMMERMAN S. Arthroscopic Treatment of Anterior-Inferior Glenohumeral Instability. The Journal of Bone and Joint Surgery-American Volume. 2000;82(7):991-1003.
Marquardt B, Witt K, Liem D, Steinbeck J, Pötzl W. Arthroscopic Bankart Repair in Traumatic Anterior Shoulder Instability Using a Suture Anchor Technique. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2006;22(9):931-936.
Flinkkilä T, Knape R, Sirniö K, Ohtonen P, Leppilahti J. Long-term results of arthroscopic Bankart repair: Minimum 10 years of follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;26(1):94-99.
Plath J, Aboalata M, Seppel G, Juretzko J, Waldt S, Vogt S et al. Prevalence of and Risk Factors for Dislocation Arthropathy. The American Journal of Sports Medicine. 2015;43(5):1084-1090.
KIM S, HA K, CHO Y, RYU B, OH I. ARTHROSCOPIC ANTERIOR STABILIZATION OF THE SHOULDER. The Journal of Bone and Joint Surgery-American Volume. 2003;85(8):1511-1518.
Gerometta A, Rosso C, Klouche S, Hardy P. Arthroscopic Bankart shoulder stabilization in athletes: return to sports and functional outcomes. Knee Surgery, Sports Traumatology, Arthroscopy. 2014;24(6):1877-1883.
Rahme H, Vikerfors O, Ludvigsson L, Elvèn M, Michaëlsson K. Loss of external rotation after open Bankart repair: an important prognostic factor for patient satisfaction. Knee Surgery, Sports Traumatology, Arthroscopy. 2009;18(3):404-408.
Weel H, Tromp W, Krekel P, Randelli P, van den Bekerom M, van Deurzen D. International survey and surgeon’s preferences in diagnostic work-up towards treatment of anterior shoulder instability. Archives of Orthopaedic and Trauma Surgery. 2016;136(6):741-746.
Leroux T, Saltzman B, Meyer M, Frank R, Bach B, Cole B et al. The Influence of Evidence-Based Surgical Indications and Techniques on Failure Rates After Arthroscopic Shoulder Stabilization in the Contact or Collision Athlete With Anterior Shoulder Instability. The American Journal of Sports Medicine. 2016;45(5):1218-1225.
Habermeyer P, Gleyze P, Rickert M. Evolution of lesions of the labrum-ligament complex in posttraumatic anterior shoulder instability: A prospective study. Journal of Shoulder and Elbow Surgery. 1999;8(1):66-74.
Burkhart S, De Beer J. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2000;16(7):677-694.
Boileau P, Villalba M, Héry J, Balg F, Ahrens P, Neyton L. Risk Factors for Recurrence of Shoulder Instability After Arthroscopic Bankart Repair. The Journal of Bone & Joint Surgery. 2006;88 (8):1755-1763.
Kim K, Saper M. Postoperative Management Following Arthroscopic Bankart Repair in Adolescents and Young Adults: A Systematic Review. Arthroscopy, Sports Medicine, and Rehabilitation. 2020;2(6):e839-e845.
McIsaac W, Lalani A, Silveira A, Chepeha J, Luciak-Corea C, Beaupre L. Rehabilitation after arthroscopic Bankart repair: a systematic scoping review identifying important evidence gaps. Physiotherapy. 2022; 114:68-76.
Kim S, Ha K, Jung M, Lim M, Kim Y, Park J. Accelerated rehabilitation after arthroscopic bankart repair for selected cases: a prospective randomized clinical study. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003;19(7):722-731.
Wilson K, Popchak A, Li R, Kane G, Lin A. Return to sport testing at 6 months after arthroscopic shoulder stabilization reveals residual strength and functional deficits. Journal of Shoulder and Elbow Surgery. 2020;29(7):S107-S114.
Memon M, Kay J, Cadet E, Shahsavar S, Simunovic N, Ayeni O. Return to sport following arthroscopic Bankart repair: a systematic review. Journal of Shoulder and Elbow Surgery. 2018;27 (7):1342-1347.