Research - (2022) Volume 17, Issue 6
Graston Technique Versus Soft Tissue Release on Myofascial Neck Pain Syndrome: A Randomized Controlled Trial
Mohamed Serag Eldein Mahgoub1, Neveen Abdelatif Abdelraouf2*, Mohamed Ali Elshafey3, Mohamed T Eldesoky4, Sobhy Mahmoud Aly5, Samah Saad Zahran6 and Enas E. Abutaleb7*Correspondence: Neveen Abdelatif Abdelraouf, Basic Sciences department-Faculty of Physical Therapy-Cairo University, Egypt, Tel: 00201140974442, Email:
2Basic Sciences department-Faculty of Physical Therapy-Cairo University, Egypt
3Department of Physical Therapy for Pediatrics- Faculty of Physical Therapy-Cairo University, Egypt
4Basic Sciences department-Faculty of Physical Therapy. Cairo University, Egypt, and Faculty of Applied Medical Sciences, University of Tabuk, Saudi Arabia
5Department of Biomechanics, Faculty of Physical Therapy, Cairo University, Cairo, Egypt
6Department of Musculoskeletal Disorders and their Surgery, Faculty of Physical Therapy, Cairo University, Egypt
7Basic Sciences department- Faculty of Physical Therapy-Cairo University and Heliopolis University, Egypt
Received: 18-Nov-2022 Accepted: 20-Dec-2022 Published: 20-Dec-2022
Abstract
Background: Myofascial Pain Syndrome (MPS) is a local pain disease affecting all ages that are characterized by trigger points (TrPs) in muscles or fascia.
Objective: To compare the efficacy of the Graston technique versus soft tissue release on patients with myofascial neck pain syndrome.
Design: pre-test post-test randomized controlled trial.
Participants: 60 (male and female) Patients ages ranged from 25 to 40 years assigned to 3 groups.
Interventions: Each group consists of 20 cases Group (A) received Graston technique plus conventional treatment. Group (B) received soft tissue release plus conventional treatment. Group (C) received traditional treatment only.
Main Outcome Measures: They were assessed for cervical pain intensity using analogue visual scale, daily activities using a neck disability score, range of motion using an inclinometer, and tenderness using a pressure algometer pre-and post-treatment.
Results: There was a significant difference between the Graston technique and soft tissue release. Both were more successful than the control group in pain relief, functional impairment, and range of motion, with the Graston approach having a more beneficial impact.
Conclusion: Graston technique has a superior impact on relieving neck discomfort, functional impairment, and range of motion.
Keywords
Graston technique. Soft tissue release. Myofascial neck pain syndrome.
Introduction
MPS symptoms can develop as a result of muscular overuse or injury, although some individuals have no triggering reasons(1). The onset of pain may be acute or insidious (1). Directly pathoanatomic caused MNP, which is rarely identifiable, might be associated with degenerative process or pathology identified throughout diagnostic imaging; tissues which caused NP till now are unknown.(2)
Recently, increased recurrence and chronicity NP rates. Most NP cases did not experience complete resolution of the symptom, from 50% to 85%, whose experience NP noted again post one-two later. (3)
Graston technique is a supplementary modality and could aid in the delivery of several manual therapy techniques (4)
Instrument edges and points would ride over soft tissues as stylus does a record groove giving "feedback," and cases had unique sensations when palpated with tools, such as " numb, crunchy, itchy, warm, or painful," which could help clinician (5)
Graston technique is believed to stimulate connective tissues remodeling through resorption of excessive fibrosis and inducing repair and regeneration of collagen secondary to fibroblast recruitment. Where released and breakdown of scar tissues, adhesions, and fascial restriction. (6)
Soft tissue release (STR) is a therapeutic strategy, treatment, and rehabilitation tool, as well as hands-on therapy, in which pressure exerted by therapist hands to and into the client's body. (7)
STR is leading therapy that involves communication between therapist and patients and actively promotes feedback on treatment responses and body awareness.
The STR technique has many interdependent components. Soft tissue rebounding makes up one of the manual applications of procedures, while soft tissue unwinding makes up the third. Three pieces come together to form a triangle. Setting goals for every component of the triangle as a therapist and connecting with the client, and getting their input are the two parts (8).
Study design
A randomized controlled study including a pre and post-test. The techniques used were approved by the Institutional Ethical Committee, and signed informed permission was obtained from the case. n. PACTR (202008747287742). Participants Our investigation was performed in Cleopatra group hospitals from December 2019 to May 2020 to compare the effect of the Graston method VS. soft tissue release on myofascial neck pain syndrome.
Randomization
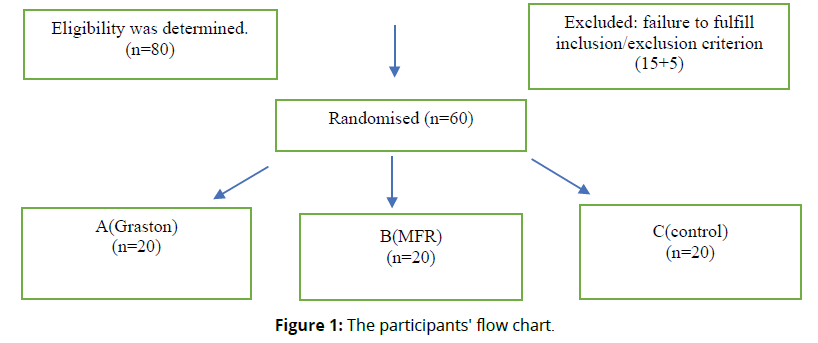
Eligibility was determined for 80 individuals. Sixty patients were allocated to three groups, as shown in Figure 1 (Figure 1). Using a computer randomization tool, simple selection was employed to allocate cases to three groups of equal numbers.
Intervention
This research included 60 male and female patients aged 25 to 40 with mechanical neck discomfort. An orthopedic physician in charge of diagnosing cases based on clinical and radiographic assessment assigned all participants. They participated after providing signed consent permission.
Inclusion criteria: Age around 25 and 40 years, a history of chronically (for at least 90 days), clinically confirmed myofascial neck pain syndrome (MNPS) among both genders with no referred pain, spinal arthritis, or discs collapse, and sufficient comprehension to execute the tests.
Exclusion criteria: A history of infectious illness and systemic problems such as diabetic, hematologic disease, rheumatoid arthritis, cancer patients, stroke, severe cardiac disease, and deaf and blind individuals
They were divided into equal three class at random. The Graston procedure was used on 20 patients in Group A, and standard treatments included (hot packs, TENS, exercises &US). Soft tissue release and standard therapy were administered to 20 individuals in Group B. Only standard treatment was used on the 20 individuals in Group C.
Procedures for Evaluation
Each patient was evaluated both before and after therapy. The analogue visual scale was used to evaluate pain (9). The Neck Disability Score Survey was created to provide data like how neck pain affects capabilities and management (10),
Algometer to measure pressure pain threshold (11), and an inclinometer to assess range of motion. The Deluxe Inclinometer has a three-inch display with one-degree markings. (12) .
Transparent Grading Sheet
This sheet was used to locate trigger points (TrPs) and guarantee the exact application of manual techniques to the same target point during the treatment sessions (13).
Procedures for treatment
Soft tissue mobilization with the use of an instrument
Procedures: All participants were notified among all techniques prior they began.
Group A: consisted of 20 patients with MNPS who got the Graston method as well as standard therapy. Put lubricating substance to the treatment region while the patient is seated comfortably on a stool. Perform IASTM at degrees (30-60) for 40 to 120 seconds on each side till redness arises; use cold packs following procedure to reduce redness. (14)
Group B: 20 patients received soft tissue release &conventional treatment
Cross-Hand Release of Lateral Neck
The client's head and neck should be moved away from the treating sides when patients had to lie supine without a pillow, with the arm and wrist straight, the arm externally rotated at the shoulder joint, and the palm was pointing upward. Sit or stand at the treatment table's corner, edge, or top. Put one hand on the patient's chest, so the palm touches the collarbone, and the fingers point toward the patient's elbow on the same side. Place the other hand beneath the patient's jaw, using it as a handle and pointing the fingers toward the top of the patient's head. Lean through the barrier between the casing and the tissue depth and follow each delicate release in three dimensions. The process was carried out for at least five minutes (15).
Group C (Control group)
Twenty patients got just standard therapy (US, hot packs, and TENS) as well as proprioceptive and isometric neck exercises. For four weeks, therapeutic sessions took place three times each week.
Sample size calculation
Preliminary power analysis was conducted using G*Power 3.1.9.2 software to prevent a type II error with the following parameters [power (1−α error P) = 0.95, α = 0.05, effect size = 1.187]. Analysis was determined as a sample size of 60 individuals divided into three groups (20 each). For this calculation, we used pain intensity as the primary outcome measure in 15-subject pilot research.
Results
Our target was to investigate Graston technique versus soft tissue release on myofascial neck pain syndrome. Sixty patients aged 25 to 40 were randomly allocated into three groups to contribute to our investigation. Data was acquired from the three Classes concerning analogue visual scale, pressure algometer from right and left upper trapezius muscles, neck disability index, and neck range of motion estimated at start and after therapy for all classes. SPSS for Windows version 25 was used to do statistical analysis and comparisons on the parameters.
Normality test
The statistical measures were uniformly distributed according to the Shapiro- Wilk test (p >0.5).
Table 1 demonstrates the starting demographic profile of the individuals. No significant differences were observed among studied cases regarding age, weight, height, or BMI (p>0.05) (Table 1).
| Characteristics | Group I (n=20) | Group II (n=20) | Group III (n=20) | F | P |
|---|---|---|---|---|---|
| Age(years) | 31.88±4.84 | 32.67±5.55 | 34.07±5.11 | 0.7 | 0.51 |
| Weight(kg) | 75.87±9.25 | 74.33±10.22 | 80.07±13.09 | 1 . 1 | 0,34 |
| Height(m) | 1.66±0.09 | 1.70±0.08 | 1.68±0.08 | 0,85 | 0,43 |
| BMI (kg/m2) | 27.2±4.13 | 25.60±4.08 | 28.00±5.28 | 1,09 | 0,35 |
| Kg; kilogram; m, meter, BMI. Body mass Index; F, fisher test; p, the probability value | |||||
Results of Mixed design multivariate analysis of Variance (MANOVA): Mixed design multivariate analysis was done for assessment differentiation among cases in the studied groups in changing in scores on results., Wilk's A = 0.19, F (17,10) = 6.01, P< 0.0001, ƞ2 = 0.59, for time, Wilk's A = 0.019, F (8,40) = 244.61, p < 0.0001, ƞ2 = 0.97, and interplay among groupings and times, Wilk's A= 1. 51, F (17,23) = 13.11, p < 0.0001, ƞ2 = 0.81.
Results of Mixed design analysis of Variance (ANOVA): Significantly changing on VAS outcome variable, F(2,55) = 42.17, p< 0.0001, ƞ2 = 0.71, for Right trapezius pressure algometer outcome variable, F(2,55) = 56.17, p< 0.0001, ƞ2 = 0.73, for left trapezius pressure algometer outcome variable, F(2,42) = 49.93, p< 0.0001, ƞ2 = 0.704 for neck disability score outcome variable, F(2,55) = 67.22, p< 0.0001, ƞ2 = 0.81, for flexion ROM outcome variable, F(2,55) = 109.33, p< 0.0001, ƞ2 = 0.90, for extension ROM, F(2,55) = 13.21, p< 0.0001, ƞ2 = 0.41, for right lateral flexion ROM outcome variable, F(2,55) = 7.34, p= 0.004, ƞ2 = 0.31, and for left lateral flexion ROM outcome variable, F(2,55) = 9.75, p< 0.0001, ƞ2 = 0.37.
Within-group comparison: As shown in Table 2, there is a significant difference in all findings between before and after treatments in each group.
Measure |
Groups | (I) time | (J) time | M D (I-J) | SE | Sig. b | 95% CI b |
|---|---|---|---|---|---|---|---|
| VAS (mm) | Graston | 1 | 2 | 5.40* | 0.226 | 0.0001 | 4.94, 5.86 |
| STR | 1 | 2 | 4.07* | .226 | 0.0001 | 3.61, 4.52 | |
| traditional | 1 | 2 | 2.53* | .226 | 0.0001 | 2.08, 2.99 | |
| Rt Trap | Graston | 1 | 2 | -4.33* | .144 | 0.0001 | -4.62, -4.04 |
| STR | 1 | 2 | -2.30* | .144 | 0.0001 | -2.59, -2.01 | |
| traditional | 1 | 2 | -1.00* | .144 | 0.0001 | -1.29, -0.71 | |
| Lt Trap | Graston | 1 | 2 | -4.38* | .131 | 0.0001 | -4.65, -4.12 |
| STR | 1 | 2 | -2.08* | .131 | 0.0001 | -2.35, -1.82 | |
| traditional | 1 | 2 | -0.97* | .131 | 0.0001 | -1.23, -0.70 | |
| NDI | Graston | 1 | 2 | 18.93* | .744 | 0.0001 | 17.43, 20.43 |
| STR | 1 | 2 | 13.47* | .744 | 0.0001 | 11.97, 14.97 | |
| traditional | 1 | 2 | 4.53* | .744 | 0.0001 | 3.03, 6.03 | |
| Flex(deg). | Graston | 1 | 2 | -32.00* | 1.412 | 0.0001 | -34.85, -29.15 |
| STR | 1 | 2 | -15.33* | 1.412 | 0.0001 | -18.18, -12.48 | |
| traditional | 1 | 2 | -2.33 | 1.412 | 0.11 | -5.18, 0.52 | |
| Ext(deg). | Graston | 1 | 2 | -12.00* | 1.059 | 0.0001 | -14.14, -9.86 |
| STR | 1 | 2 | -9.33* | 1.059 | 0.0001 | -11.47, -7.20 | |
| traditional | 1 | 2 | -3.67* | 1.059 | 0.001 | -5.80, -1.53 | |
| Rt Side Bending(deg) | Graston | 1 | 2 | -14.04* | .823 | 0.0001 | -15.11, -12.21 |
| STR | 1 | 2 | -7.01* | .823 | 0.0001 | -8.64, -5.36 | |
| traditional | 1 | 2 | -6.54* | .823 | 0.0001 | -8.19, -5.22 | |
| Lt Side Bending(deg) | Graston | 1 | 2 | -13.68* | .890 | 0.0001 | -15.47, -11.88 |
| STR | 1 | 2 | -5.00* | .890 | 0.0001 | -6.79, -3.21 | |
| traditional | 1 | 2 | -7.11* | .890 | 0.0001 | -8.37, -5.62 | |
| P value: adjusted to Bonferroni Post Hoc | |||||||
Between-group comparison: It is explained in table 3.
Measure |
(I) Groups | (J) Groups | MD (I-J) | SE | Sig. | 95% CI |
|---|---|---|---|---|---|---|
| VAS(mm) | Graston | STR | -18.00* | 3.4 | 0.0001 | -26.4, -9.6 |
| Traditional | -30.67* | 3.4 | 0.0001 | -39.1, -22.3 | ||
| STR | Traditional | -12.67* | 3.4 | 0.002 | -21.1, -4.3 | |
| Rt Trap | Graston | STR | 2.30* | 0.35 | 0.0001 | 1.44, 3.17 |
| Traditional | 3.63* | 0.35 | 0.0001 | 2.77, 4.5 | ||
| STR | Traditional | 1.33* | 0.35 | 0.001 | 0.468, 2.2 | |
| Lt Trap | Graston | STR | 2.55* | 0.37 | 0.0001 | 1.63, 3.47 |
| Traditional | 3.60* | 0.37 | 0.0001 | 2.68, 4.52 | ||
| STR | Traditional | 1.050* | 0.37 | .021 | 0.13, 1.97 | |
| NDI | Graston | STR | -5.40* | 1.5 | 0.002 | -9.13, -1.67 |
| Traditional | -16.80* | 1.5 | 0.0001 | -20.53, -13.07 | ||
| STR | Traditional | -11.40* | 1.5 | 0.0001 | -15.13, -7.67 | |
| Flex(deg). | Graston | STR | 16.00* | 1.76 | 0.0001 | 11.62, 20.38 |
| Traditional | 25.67* | 1.76 | 0.0001 | 21.28, 30.05 | ||
| STR | Traditional | 9.67* | 1.76 | 0.0001 | 5.28, 14.05 | |
| Ext(deg). | Graston | STR | 2.33 | 2.00 | 0.75 | -2.65, 7.31 |
| Traditional | 9.67* | 2.00 | 0.0001 | 4.69, 14.65 | ||
| STR | Traditional | 7.33* | 2.00 | .0020 | 2.35, 12.31 | |
| Rt Side Bending(deg) | Graston | STR | 5.00* | 1.66 | .0130 | 0.87, 9.13 |
| Traditional | 5.33* | 1.66 | 0.007 | 1.21, 9.46 | ||
| STR | Traditional | 0.33 | 1.66 | 1.000 | -3.8, 4.46 | |
| Lt Side Bending(deg) | Graston | STR | 5.33* | 1.52 | 0.003 | 1.56, 9.11 |
| Traditional | 6.00* | 1.52 | 0.001 | 2.22, 9.78 | ||
| STR | Traditional | 0.67 | 1.52 | 1.000 | -3.11, 4.45 | |
| P value: adjusted to Bonferroni Post Hoc | ||||||
Discussion
The current study included 60 individuals suffering from myofascial neck pain condition. Their ages ranged from twenty-five to forty years, separated into three equal Classes. All patients were evaluated before and after the trial using analogue visual scale, neck disability score, inclinometer, and algometer.
Pain, right and left upper trapezius pressure algometry, neck disability score, and neck range of movements data reported statistically significant differences between groups (P<0.05). Graston technique is most effective than soft tissue release &traditional treatment. These findings align with Kim J et al., 2017 who found improved function post-IASTM (16). That caused improving in muscles activities levels. This might depend on improving performances throughout daily activity and ultimately reducing one's disability levels. (16).
Furthermore, our findings are consistent with the findings of Motimath et al., 2017 who deduced that the IASTM method using the M2T razor is a crucial asset that can reduce pain instantly in individuals with upper trapezius spasm; users examined the impact of the M2T razor on individuals with neck pain and discovered a significant decline in pain level as well as enhanced level of activity, and they demonstrated that M2T razor could be utilized to loosen rigid fascia by applying rhythmic strokes over the fascia till the adhesions and crosslinkages are broken, and the release of the fascia occurred(17).
Kojidi et al., 2016 found that passive treatments for 90 seconds or 20 seconds of active treatments for cases with myofascial TPs in upper trapezius muscles led to a significant decreasing in myofascial TPs sensitivities, increasing muscle fibers flexibilities, and improving ROM. (18)
In the present study, our choice to use the Graston technique was supported by Hammer et al., 2008 & Baker et al., 2015 (19,6); they reported that improvement in the Graston group might be related to IASTM and improving soft tissues extensibilities by treating its restriction.
Graston technique has advantages over other soft tissue mobilization where metal surface of the instrument does not compress tissues, as do finger fat pads (20). The Graston group's findings are consistent with the findings of Cheatham et al. 2016, who observed increased function following IASTM. (20) Because pain-relieving therapies may enhance neck function, a drop in NDI scores may be ascribed to pain relief.
Consequently, both techniques were useful individually in increasing ROM, reducing pain, and improving function; however, when we compared the effectiveness of both methods, there was no statistically significant difference in improving any of the outcome variables.
Similar results were mentioned in previous research by Paranjape 2020, who reported that manual STM and IASTM have advantages and disadvantages. Manual STM does not need any specific instrument for treatment application; however, it can cause increased joint stress in the hands. A survey reported that 91% of absenteeism was attributed to pain in the therapist's hands due to manual STM. (21)
According to Snodgrass et al., 2003, the Graston approach necessitates the use of tools as well as expertise in its application. The IASTM equipment is an ergonomically built instrument that glides across adherent tissues and reverberates sensation in our hands, allowing us to pinpoint specific regions of limitation and cure them. (22) It alleviates the therapist's induced tension. Our research, on the contrary, disagrees with a systematic review by Nazari et al., 2019, which also doesn't confirm the use of IASTM to enhance discomfort, functioning, or range of motion in people not having extremities or spinal disorders or those who have a variety of diseases. (23). Even though the Graston approach was shown to be a more effective overactive therapy in this trial, it did not achieve a statistically significant difference compared to other therapies. This is achievable due to the easy posture; Graston is a practical and simple procedure. (24).
Concerning the result of the soft tissue release group, our study's result agrees with Nitsure P & Welling A.,2014, who reported that determining Gross MFR effects on upper limb and neck with mechanical NP for reducing pain and improving functional ability (25).
Our results align with Gauns & Gurudut 2018 who stated that the MFR technique affects chronic non-specific NP on 30 subjects, and MFR is an effective manual therapy technique for reducing pain and disability and improving isometric extension strength of the neck in patients with non-specific chronic neck pain. (26) Despite MNPS prevalence, there was a massive gap in previous investigations that failed to provide sufficient, conclusive evidence favoring one specific intervention over another in conservative pathology treatments. Based on earlier inquiries on the present practice patterns, 3 appears to be a cohort of subjects with NP who respond favorably to mobilization/ manipulation combination, exercise, and possibly traction interventions (2).
Cleland and colleagues 2007, researched cervical radiculopathy cases; they reported a drastic reduction in disability following conservative management strategies, including intermittent cervical traction and deep neck flexor muscles strengthening. (27)
Conclusion
In terms of lowering myofascial neck discomfort, tenderness, and enhancing cervical range of motion and daily living activities, the Graston approach outperforms soft tissue release and conventional therapy.
Competing Interests
No competing interests
Funding
self-funding.
Author's contributions
7 authors contributed to this investigation and all requirements for our research.
References
Tantanatip A, Chang KV. Myofascial Pain Syndrome. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020.
Childs JD, Cleland JA, Elliott JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008; 38: A1– A34.
Kenneth Olson. The Cervical Spine. Chapter 6 In: Olson, K. Manual Physical Therapy of the Spine. Elsevier, 2015
Chaitow, L Fascial Dysfunction, Manual Therapy Approaches. Handspring, Edinburgh. (Chapter 12 is dedicated to IASTM, authored by Warren Hammer), 2014
Myers, T Anatomy Trains, Myofascial Meridians for Manual and Movement Therapists, 3rd Ed. Churchill Livingstone, Edinburgh. (Excellent conceptualization of the Kinetic Chain), 2014
Baker RT, Hansberger BL, Warren L, et al. A novel approach for the reversal of chronic apparent hamstring tightness: a case report. Int J Sports Phys Ther. 2015;10(5):723–733
Christopher H. Wise .Orthopaedic Manual Physical Therapy: From Art to Evidence Section 2: Soft Tissue Approaches. 2015.
Michael Stanborough. Direct Release Myofascial Technique - An Illustrated Guide for Practitioners 98-99 Pages . 1st edition.2004.
Dimitriadis, Z., Strimpakos, N., Kapreli, E., and Oldham, J. Validity of visual analog scales for assessing psychological states in patients with chronic neck pain. Journal of Musculoskeletal Pain, 2014, 22(3), 242–246
Gay RE, Madson TJ, Cieslak KR. "Comparison of the Neck Disability Index and the Neck Bournemouth Questionnaire in a sample of patients with chronic uncomplicated neck pain." J Manipulative Physiol Ther. 2007 May;30(4):259-62.
Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2005: CD 004250. Youdas JW, Carey JR, Garrett TR.: Reliability of Measurements of the Cervical Spine Range of Motion - Comparison of Three Methods, Physical Therapy, February 1991.
Gomaa, E. F., Fiyaz, N. A., El-Mofty, A. O., Zaky, L. A. (2016). Effect of iliotibial band myofascial release in treatment of knee osteoarthritis. Doctoral Thesis, Faculty of Physical Therapy, Cairo University.
Howitt, S., Wong, J., & Zabukovec, S. The conservative treatment of trigger thumb using Graston techniques and active release techniques. Journal of the Canadian Chiropractic Association, 2006, 50(4), 249– 254
Gauns SVand Gurudut PV. A randomized controlled trial to study the effect of gross myofascial release on mechanical neck pain referred to upper limb. Int J Health Sci (Qassim). 2018;12(5):51-59.
Kim J, Sung DJ, Lee J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: Mechanisms and practical application. J Exerc Rehabil. 2017;13(1):12–22
Motimath B., N. Ahammed, D. ChivateImmediate effect of IASTM with M2Tblade technique in trapezitis: an experimental study J Int Appl Res, 2017 (3):527-529
Kojidi, M. M., Okhovatian, F., Rahimi, A., Baghban, A. A., & Azimi, H. Comparison between the effects of passive and active soft tissue therapies on latent trigger points of upper trapezius muscle in women: Singleblind, randomized clinical trial. Journal of Chiropractic Medicine, 2016, 15(4), 235– 242
Hammer WI. The effect of mechanical load on degenerated soft tissue. J Bodyw Mov Ther. 2008;12(3):246–56.
Cheatham, S. W., Lee, M., Cain, M., & Baker, R. The efficacy of instrument assisted soft tissue mobilization: A systematic review. Journal of the Canadian Chiropractic Association, 2016,60(3), 200– 211
Paranjape S, Lad R. Comparison of manual versus instrument assisted soft tissue mobilisation of levator scapulae in chronic neck pain. International Journal of Research and Review. 2020; 7(3): 364-369.
Snodgrass SJ, Rivett DA, Chiarelli P, et al. Factors related to thumb pain in physiotherapists. Aust J Physiother. 2003;49(4):243–50.
Nazari, G., Bobos, P., MacDermid, J. C., & Birmingham, T. The effectiveness of instrument-assisted soft tissue mobilization in athletes, participants without extremity or spinal conditions, and individuals with upper extremity, lower extremity, and spinal conditions: a systematic review. Archives of physical medicine and rehabilitation, 2019, 100(9), 1726-1751.
Loghmani, M. T., & Warden, S. J. Instrument-assisted cross-fiber massage accelerates knee ligament healing. The Journal of Orthopaedic & Sports Physical Therapy, 2009, 39, 506– 514.
Nitsure P, Welling A. Effect of gross myofascial release of upper limb and neck on pain and function in subjects with mechanical neck pain with upper limb radiculopathy:A clinical trial. Int J Dental Med Res. 2014; 1:8-16
Gauns, S. V., & Gurudut, P. V. A randomized controlled trial to study the effect of gross myofascial release on mechanical neck pain referred to upper limb. International journal of health sciences, 2018,12(5), 51.
Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2007; 89: 69-74.