Full Length Research Article - (2023) Volume 18, Issue 4
Long Term Effect Of Radial Shockwave Therapy Versus Phonophoresis In Chronic Plantar Fasciitis Randomized Controlled Stu
Maher Ahmed Elkeblawy1, Mohamed Mohamed Mashaly2* and Yasser Ramzy Lahseen3*Correspondence: Mohamed Mohamed Mashaly, Physical therapist at the National Institute of Neuromotor System, General Organization for Teaching Hospitals and Institutes, Egypt, Email:
2Physical therapist at the National Institute of Neuromotor System, General Organization for Teaching Hospitals and Institutes, Egypt
3Assistant Professor of Basic Sciences Faculty of physical therapy Cairo University, Egypt
Received: 06-Jul-2023 Reviewed: 20-Jul-2023
Abstract
Purpose: to look into the impacts of shock wave therapy versus phonophoresis in chronic plantar fasciitis.
Subjects: sixty-three patients having unilateral chronic plantar fasciitis.
Design: pre and post Randomized Control Trial.
Methods: The patients were randomly assigned to Group A who received Radial Shockwave Therapy (2000 SWs energy intensity between 0.25 and 0.35 mJ/mm) at (frequency= 10Hz) for 4 weeks 1 session per week additional to conventional treatment. Group B received ultrasound ketoprofen phonophoresis continuous mode, base frequency of 1MHz, power 2 w/cm2, applied for three minutes to each location, and conventional treatment for 4 weeks 3 sessions per week. Group C control group received traditional treatment only (night splint + foot orthosis + calf muscle /plantar fascia stretch). Pain intensity by VAS, Ultrasonography-assessed plantar fascia thickness, and lower extremity functional scale were evaluated at baseline, one month after the intervention ended, and six months later.
Results: Patients from both groups significantly improved on all assessed variables. Compared to the phonophoresis group, the shock wave group significantly improved on measures of pain, plantar fascia thickness, and lower limb functional scale.
Conclusion: from the results Group A (RSWT) and Group B (phonophoresis) exhibited more significant improvements in all variables compared to Group C (splint) in the enhancement of pain reduction, plantar fascia thickness as well as the improvement of lower extremity functional scale at the short-term follow-up one month (4 weeks) and long-termed follow-up six months in the management of patients suffering from chronic plantar fasciitis. However, the shockwave group's progress was significantly more noticeable than the phonophoresis group's (p<0.0001).
Keywords
Plantar fasciitis. Radial shockwave therapy (RSWT). Phonophoresis. Visual Analogue Scale (VAS). Ultrasonography / Ultrasound Scan. Night Splint.
Introduction
Plantar fasciitis (PF) is the most commonly diagnosed and treated foot condition in adults, and it includes inflammation of the thick band of tissue that runs across the bottom of the foot. Also, it connects the heel bone to the toes (plantar fascia) (Johnson et al., 2014).
"Plantar heel pain" is a broad term that describes various conditions that can cause discomfort on the underside of the heel bone. These conditions include PF, the presence of a bony outgrowth called a calcaneal spur, inflammation of the bursa beneath the calcaneus (subcalcaneal bursitis), inflammation of the periosteum covering the calcaneus (calcaneal periostitis), stress fractures in the calcaneus (calcaneal stress fracture), fat pad syndrome, compression or entrapment of Baxter's nerve, and nerve root irritation (radiculopathy) (Hossain & Makwana, 2011).
PF, a chronic degenerative condition resulting in medial plantar heel pain, accounts for approximately one million medical appointments annually. Those affected by plantar fasciitis commonly encounter heightened discomfort during their initial strides in the morning or after extended standing periods(Thompson et al., 2014).
PF, which affects 4%–7.0% of the community (Thomas et al., 2019), has been related to a decline in quality of life as it relates to health, which includes experiences such as social isolation, a negative perception of overall health, and limitations in functional abilities.
Sedentary middle-aged and older adults are particularly vulnerable. It is estimated that plantar fasciitis constitutes approximately 8.0% of all runningrelated injuries (Dedes et al., 2019).
Certain factors increase the risk of developing PF, including structural abnormalities causing faulty foot mechanics, degenerative changes associated with aging, being overweight, making training errors, and engaging in occupations that involve prolonged standing. People in the following fields fit this description: educators, construction workers, cooks, nurses, members of the armed forces, and athletes training for a long-distance race (Owens et al., 2013).
When comparing Ultrasound (US) to other diagnostic tools, including magnetic resonance imaging (MRI), Ultrasound has been proven to be the most accurate and reliable. The overall advantages of the US, such as its low cost, simple administration, lack of invasiveness, and few contraindications, make it the best diagnostic modality for PF. Therefore, considering the effectiveness of the US in diagnosing PF and accurately tracking improvements resulting from rehabilitation interventions, its incorporation into rehabilitation clinics should be strongly considered (Ahn et al., 2016).
It has been observed that ultrasonography measurements indicating a thickness exceeding 4 mm can be considered significant for diagnostic purposes (Abul et al., 2015).
Conservative and surgical methods are both viable choices for treating PF. Night splints, orthotics, cast immobilization for 4–6 weeks, nonsteroidal antiinflammatory drugs (NSAIDs), corticosteroid injections, stretches, and physical therapy are all examples of conservative therapies. Laser therapy, US therapy, iontophoresis, and extracorporeal shock wave therapy are frequently applied physical therapy techniques for PF. An operation is usually only considered a last resort when a year or more has gone since the disease's initial diagnosis and when more conservative treatments have been ineffective (Dedes et al., 2019).
shock wave (SW) therapy has developed to deal with long-standing tendon problems effectively. SW therapy is a technique used to treat chronic illnesses by applying shock waves to the body via pressurised air or electromagnetic pulses. Extracorporeal shock waves were first reported as being used to treat plantar fasciitis in the mid-1990s (Simplicio et al., 2020).
Additionally, it has been suggested that SW can generate free radicals near cell membranes, which in turn can trigger the release of pain-reducing substances in the vicinity of the cells. Another mechanism of pain relief attributed to SW is its ability to enhance revascularization, promoting improved blood flow to the affected area. Several authors have reported that SW can induce cell apoptosis, stimulate angiogenesis (the formation of new capillaries from existing blood vessels), speed up the healing of wounds as well as promote the growth of new bone using radial pressure waves (Gollwitzer et al., 2013).
Therapeutic Ultrasound involves utilizing mechanical acoustic energy to treat various soft tissue conditions, such as bone fractures and dermal wounds. This type of Ultrasound can be categorized into three main types: conventional Ultrasound (CUS), low-intensity pulsed Ultrasound (LIPUS), as well as noncontact low-frequency ultrasound (NCLFUS). These different categories represent distinct spectra of therapeutic Ultrasound and are employed for specific therapeutic purposes (Bélanger & Bélanger, 2010).
The benefits of therapeutic Ultrasonography include alleviating muscle spasms and enhancing collagen fibers' extensibility. Cavitation and acoustic microstreaming are examples of the non-thermal mechanisms of Ultrasound responsible for these effects. When Ultrasound is delivered to a damaged area, bubbles filled with gas are pushed into the interstitial fluid and then form, oscillate, and pop. This process is known as cavitation. Cavitation has a crucial role in facilitating acoustic microstreaming. As a result, microstreaming modifies the membrane shape, function, and permeability, boosting cellular activity and promoting tissue repair. The positive effects of ultrasound therapy are due to the enhanced cellular activity triggered by ultrasound energy (Johns, 2002).
Phonophoresis is a type of therapeutic US that uses mechanical waves of a very high frequency to cause vibration. Tissues are heated intensely due to the vibrations. Using this energy source to generate deep heat has been shown to boost local blood flow, alleviate pain, as well as aid in the resolution of fibrosis (Gonnade et al., 2018).
Although numerous studies have shown that SW reduced pain as well as increased functionality in the short& medium term following treatment, its long-term effectiveness has yet to be proved (Chuckpaiwong et al., 2009) (Chuckpaiwong et al., 2009) (Morrissey et al., 2021) with a focus on PF that has returned.
Previous research has shown that SW and Ultrasound can help with PF (Al- Siyabi et al., 2022, D'Andréa Greve et al., 2009, Dedes et al., 2019). Research comparing SW with phonophoresis has not been done before.
Hence, our study was planned to compare RSWT vs. phonophoresis to provide a base for designing a rehabilitation program and finding the best and cheaper treatment for plantar fasciitis.
Delimitations
This study was delimited to the following:63 patients with chronic plantar fasciitis referred to be taking part in this study with BMI less than 30 kg/m2
• Visual analogue scale to assess pain intensity, Ultrasonography to assess plantar fascia thickness, and Lower extremity functional scale assessment of function.
• Measures were taken before and after treatment (1 month and 6 months after)
• Data was manipulated by descriptive analysis as well as inferential statistics.
• All tests were performed with a 0.05 significance level.
Materials and Methods
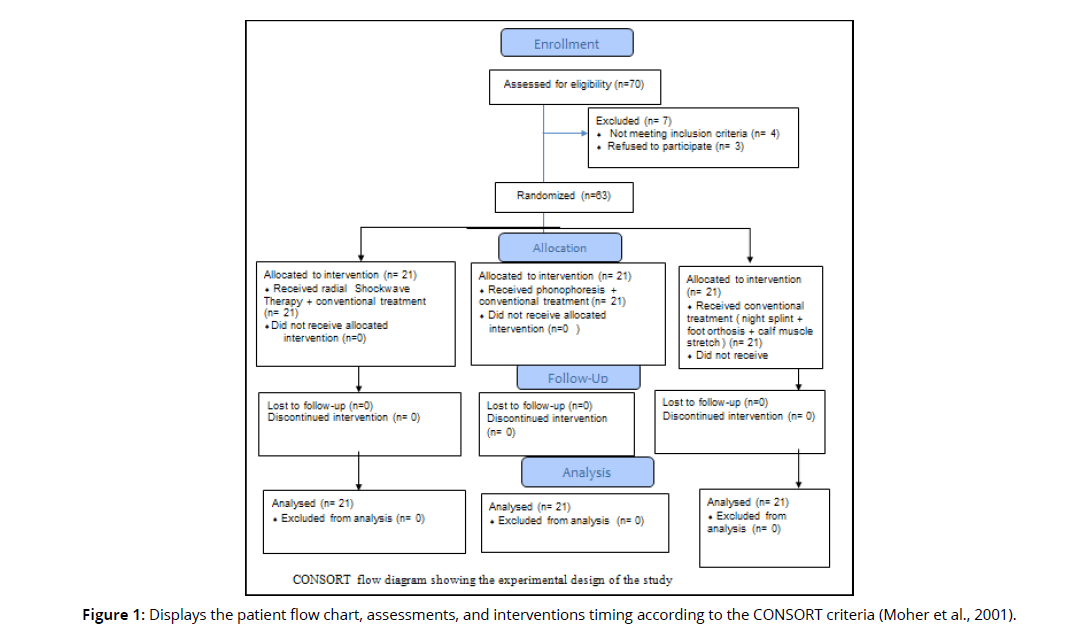
This was an interventional, randomized, controlled trial planned for six months (Figure 1). The research was conducted at the Shubrakhit General Hospital's outpatient clinic in Behira between August 2020 and December 2021. The clinical trial registration number was (no: P.T.REC/012/002482) Cairo University and Pan African Clinical Trial Registry PACTR202203539689555. All human participants were treated ethically and in compliance with the principles outlined in the World Medical Association's Declaration of Helsinki. Everyone who participated in the study signed an informed consent form after being briefed on the study's goals, assessments, and procedures.
Subjects
A total of 63 patients with chronic, unilateral PF were enrolled, all of whom had been referred to the researchers by an orthopedic physician. The patients were split into three groups, each with 21 people in it at random. The eligibility criteria included: A clinical diagnosis of PF, One-sided plantar heel pain persisting longer than six months, and Males and females aged 30-60 with a morning pain score of at least 2 on a numeric pain rating scale during the preceding week. The exclusion criteria were A history of previous surgery in lower limbs, Potential contraindications to shockwave or phonophoresis, exhibiting at least two neurologic symptoms related to root compression of the nerve before receiving conservative treatment for PF (i.e., physiotherapy, acupuncture, Therapeutic Massage, chiropractic treatment, or steroids injected locally) and also had a duration of PF of less than 4 weeks, obesity BMI>30 kg/ m-foot deformity, foot skeletal deformities, chronic diseases, and pregnancy.
Sample size calculation
G*POWER was used to determine the total number of people who took part (version 3.1.9.2; Universitat Kiel, Germany) Previous research indicated that 21 people should be included in each group. The calculations were performed using alpha= 0.05, power 80%, also effect size 0.40.
Randomization, Allocation
• The participants were randomly assigned in permuted blocks using a computer-generated randomization list created by a statistician who had no role in the recruitment process. Allocation to each treatment group was done secretly using a computer-generated random list and sealed envelopes by a staff member who was not otherwise engaged in the study's testing or treatment of participants (Figure 1).
Group A: Twenty-one patients received radial Shockwave Therapy in addition to conventional treatment For 4 weeks 1 session per week. (Grecco et al., 2013).
Group B: Twenty-one patients received ultrasound ketoprofen phonophoresis and conventional treatment for 4 weeks 3 sessions per week(R. L. Martin et al., 2014a).
Group C: Control group, twenty-one patients received conventional treatment only in the form of ( night splint + foot orthosis + calf muscle /plantar fascia stretch )(J. E. Martin et al., 2001).
Outcome Measures
Weight and height scales were used to evaluate all eligible participants' body height (cm) and weight (kg). The primary outcome of this research was pain intensity, while secondary outcomes included Ultrasonography-measured plantar fascia thickness as well as lower extremity functional scale. These secondary outcomes were assessed before the intervention began, one month after it ended, and six months later.
Visual Analogue Scale
Patients were given a VAS from 0 (no pain) to 10 to score their pain before, during as well as after physical activity (10-indescribable pain)(Laurent & Leung, 2006).
Ultrasonography
We standardized our measurements of the plantar fascia by taking them all at the point where it attaches to the anterior aspect of the inferior border of the calcaneus. A radiologist used Mindray DC-6 with a linear transducer of 7.5 and 10 MHz to measure fascia thickness. The plantar fascia was measured for thickness with the patient supine and their foot dangling off the bed (Ahn et al., 2016).
Lower Extremity Functional Scale (LEFS)
The LEFS is a self-report questionnaire. Twenty common tasks were assessed by asking patients, "Today, do you or would you have any difficulties at all with?" (Alnahdi et al., 2016).
Interventions
The conventional rehabilitation program, which included health education for the patient, was provided to all patients (weight and activity control-Night splint-Foot orthosis), plantar fascia, and gastrocnemius muscle stretching exercise.
Group A Radial shockwave therapy (RSW): The patient's knees and hips were kept in a neutral position, and they were positioned so that their feet hung off the end of the exam table. The therapist then applied clinical pressure to the calcaneus medial tuberosity & 2 cm distal to the tuberosity, where the pain was the worst. A coupling gel has been used to begin preparing the treatment area so that fewer shockwaves would be lost between the applicator tip as well as the skin. BTL-5000 SWT POWER equipment was used with a power handpiece transducer; Each patient received 2000 SWs (energy intensity of between 0.25 and 0.35 mJ/mm) at (frequency= 10Hz) (Loske, 2017).One session per week for 1 month with one-week intervals Group B Receive ultrasound phonophoresis + conventional treatment. The individual was lying supine with their knees extended. The therapist palpated the area of highest tenderness. The Chattanooga Intelect® Mobile Combo Dual Ultrasound Device and ketoprofen gel were used, with the following settings for each area being treated: continuous mode, base frequency of 1MHz, power 2 w/cm2 for a total of 3 minutes (calcaneus medial tuberosity as well as on the 2 cm distal to tuberosity) (J. E. Martin et al., 2001)
Group C (control group) Conventional treatment Night splint The night splint was secured around the foot and lower leg using Velcro straps. Patients were given instructions on how to put on the orthosis and were told to wear it while they slept. Patients were informed of potential issues and symptoms that could arise from splint use (temporary numbness of the toes, trouble with sleep, etc.). Patients who reported these issues were instructed to readjust their straps to reduce dorsiflexion of the MTP joints Foot orthosis The correct sized orthosis was chosen for each participant, and the orthoses were then inserted into the shoes. The investigator made adjustments in the clinic if any patients complained of pain. Calf muscle stretch (for one month) (Silbernagel et al., 2020). subjects were shown how to stand while performing the Achilles tendon stretching exercise properly. The stretches were instructed to be done standing, resting against the wall, while the injured leg was put behind the uninjured one. Subjects must place a bent knee in front of a straight knee with a planted heel. The stretching consisted of five sets of 20 sec. of stretching followed by 20 sec. of rest. The stretch was done twice daily, five days a week, for four consecutive weeks. The therapist kept an eye on the home program by contacting patients every week.
Stretching exercises for plantar fascia
Patients were told to sit down while crossing the affected leg over through the unaffected leg. Self-stretching the MTP joints mostly on the affected side and bringing the toes up towards the shin was recommended for patients with plantar fasciitis to achieve a stretched sensation in the sole of the foot. The pull of the plantar fascia could be felt in the opposite foot as the stretch was applied. The patient's heel was pulled with the other hand; an extra longitudinal stretch was put on the plantar: calf stretch exercise. Plantar fascia stretch exercise. They were instructed to perform ten sets of each stretch, holding each position for ten sec. The instructions instructed patients to achieve the treatments three times daily.
Data collection
Homogeneity of variance and tests for normality were performed on the data. The results of the Shapiro-Wilk test indicated that the data were not normally distributed (P<0.05) after the outlying data points were eliminated using box and whisker plots. Furthermore, there was a statistically substantial dissimilarity among groups based on Levene's test to test for the similarity of variance (P<0.05). The data obtained enabled the researcher to do both parametric and non-parametric tests. Due to the lack of normality in the data, non-parametric analysis is employed.
Statistical analysis
SPSS Package, version 25 for Windows, was used for the statistical analysis (SPSS, Inc., Chicago, IL). Data is expressed numerically as mean and standard deviation for age, lower extremity functional scale, pain severity, and plantar fascia thickness variables. The Chi-square test is used to contrast the shockwave, phonophoresis, as well as splint groups concerning the categorical variables of gender and affected side. A one-way analysis of variance (ANOVA) test was used to compare age patients among shockwave, phonophoresis, and splint groups. Kruskal-Wallis H test was used to compare shockwave, phonophoresis, and splint groups initially, one month, and then six months after treatment, to compare within each group among pre-treatment, after 1-month, as well as after-6 months for lower extremity functional scale, pain severity, and plantar fascia thickness variables. Wilcoxon signed ranks test to contrast between pretreatment VS after-1 month and pre-treatment VS after-6 months within each group regarding lower extremity functional scale, pain severity, and plantar fascia thickness variables. All tests for statistical significance (P≤ 0.05) were found to be significant.
Results
Sixty-three individuals having chronic plantar fasciitis (37 men, 26 women) were involved in the recent study, and they were split evenly among three groups (21 people each). No substantial differences (P>0.05) in age (P=0.795), BMI (P=0.444), gender (P=0.422), and affected side (P=0.297) among shockwave, phonophoresis, and splint groups (Table 1).
| Items | Groups | P-value | ||
|---|---|---|---|---|
| Shockwave group (n=21) |
Phonophoresis group (n=21) |
Splint group (n=21) |
||
| Age (year) | 39.19 ±6.45 | 40.24 ±6.92 | 38.95 ±6.20 | 0.795 |
| BMI (kg/m2) | 27.16 ±2.08 | 26.71 ±1.28 | 26.43 ±2.04 | 0.444 |
| Gender (Males: Females) | 10 (47.60%) : 11 (52.40%) | 6 (28.60%) : 15 (71.40%) | 9 (42.90%) : 12 (57.10%) | 0.422 |
| Affected side (Right: Left) | 7 (33.30%): 14 (66.70%) | 12 (57.10%): 9 (42.90%) | 10 (47.60%): 11 (52.40%) | 0.297 |
| Quantitative data (age) are expressed as mean ±standard deviation (SD) and compared statistically by ANOVA test. Qualitative data (gender and affected side) are expressed as number (percentage) and compared statistically by Chi-square test. P-value: probability value P-value>0.05: non-significant |
||||
Within-group comparisons of pre-treatment, after 1-month, as well as after-6 months (time effect) for outcomes variables, revealed there were significant (P<0.05) increases in lower extremity functional scale (Table 2) among pretreatment, after-1 month, as well as after-6 months within shockwave group (P=0.0001), phonophoresis group (P=0.0001), & splint group (P=0.001). Time effect had substantially (P<0.05) decreased pain severity (Table 2) among pretreatment, after 1 month, as well as after-6 months within the shockwave group (P=0.0001), phonophoresis group (P=0.0001), & splint group (P=0.0001). Moreover, the plantar fascia thickness significantly (P<0.05) decreased during pre-treatment, after 1 month, as well as after-6 months within the shockwave group (P=0.0001) and phonophoresis group (P=0.027). Still, there was nonsignificantly (P>0.05) decrease was observed in plantar fascia thickness among pre-treatment, after 1 month, as well as after-6 months within splint group (P=0.574) (Table 2).
Variables |
Items | Groups (Mean ±SD) | P-value | ||
|---|---|---|---|---|---|
| Shockwave group (n=21) | Phonophoresis group (n=21) | Splint group (n=21) |
|||
| Lower extremity functional scale | pre -treatment | 29.05 ±6.65 | 29.52 ±11.29 | 28.29 ±10.87 | 0.743 |
| After-1 month | 51.14 ±6.15 | 41.43 ±12.52 | 35.67 ±13.64 | 0.0001* | |
| After-6 months | 56.14 ±4.00 | 53.57 ±12.32 | 41.81 ±15.78 | 0.0001* | |
| P-value | 0.0001* | 0.0001* | 0.001* | ||
| Pain severity | pre -treatment | 6.76 ±0.99 | 7.10 ±1.00 | 6.05 ±1.47 | 0.240 |
| After-1 month | 3.43 ±1.59 | 5.00 ±1.52 | 4.67 ±1.23 | 0.005* | |
| After-6 months | 1.00 ±0.27 | 2.43 ±0.97 | 3.62 ±1.28 | 0.0001* | |
| P-value | 0.0001* | 0.0001* | 0.0001* | ||
| Plantar fascia thickness | pre -treatment | 0.70 ±0.11 | 0.63 ±0.20 | 0.62 ±0.14 | 0.061 |
| After-1 month | 0.51 ±0.11 | 0.55 ±0.19 | 0.60 ±0.13 | 0.017* | |
| After-6 months | 0.49 ±0.08 | 0.54 ±0.19 | 0.58 ±0.13 | 0.013* | |
| P-value | 0.0001* | 0.027* | 0.574 | ||
| Data are expressed as mean ± standard deviation (SD); P-value: probability value; * Significant (P<0.05) | |||||
Comparisons among groups pre-treatment, after-1 month, as well as after-6 months (group effect) for outcomes variables (Table 2) showed no substantial differences (P>0.05) in lower extremity functional scale (P=0.743), pain severity (P=0.240), as well as plantar fascia thickness (P=0.061) pre-treatment. However, there were substantial differences (P<0.05) among shockwave, phonophoresis, and splint groups after-1 month and 6 months in lower extremity functional scale (P=0.0001 & P=0.0001, respectively), pain severity (P=0.005 & P=0.0001, respectively), as well as plantar fascia thickness (P=0.017 and P=0.013, respectively).
Pairwise comparisons between pre-treatment versus after-1 month and before-treatment versus after-6 months before-treatment versus after-1 month for the lower extremity functional scale are presented in (Table 3). There were substantial (P<0.05) increases in lower extremity functional scale after-1 month and after-6 months contrasted to before-treatment within the shockwave group (P=0.0001 and P=0.0001, respectively), phonophoresis group (P=0.0001& P=0.0001, respectively), as well as splint group (P=0.0001 and P=0.0001, respectively). The chronic plantar fasciitis patients who received shockwave therapy + conventional program improved higher lower extremity functional scale after 1 month and after 6-months (76.04 and 93.25%, respectively) followed by patients treated by phonophoresis therapy + conventional program (40.35 and 81.47, respectively%) and then those received splint (traditional) program (26.09 and 47.79%, respectively). These significant increases in lower extremity functional scale after-1month and after-6 months due to time effect are more favorable of shockwave therapy programs than phonophoresis and splint programs.
| Variables | Items | Before-treatment vs. After-1 month | Before-treatment vs. After-6 month | |||||
|---|---|---|---|---|---|---|---|---|
| Shockwave | Phonophoresis | Splint | Shockwave | Phonophoresis | Splint | |||
| Lower extremity functional scale | pre-treatment | 29.05 ±6.65 | 29.52 ±11.29 | 28.29 ±10.87 | 29.05 ±6.65 | 29.52 ±11.29 | 28.29 ±10.87 | |
| After-1 month | 51.14 ±6.15 | 41.43 ±12.52 | 35.67 ±13.64 | |||||
| After-6 months | 56.14 ±4.00 | 53.57 ±12.32 | 41.81 ±15.78 | |||||
| MD (change) | 22.09 | 11.91 | 7.38 | 27.09 | 24.05 | 13.52 | ||
| Improvement % | 76.04% | 40.35% | 26.09% | 93.25% | 81.47% | 47.79% | ||
| P-value | 0.0001* | 0.0001* | 0.0001* | 0.0001* | 0.0001* | 0.0001* | ||
| Pain severity | pre-treatment | 6.76 ±0.99 | 7.10 ±1.00 | 6.05 ±1.47 | 6.76 ±0.99 | 7.10 ±1.00 | 6.05 ±1.47 | |
| After-1 month | 3.43 ±1.59 | 5.00 ±1.52 | 4.67 ±1.23 | |||||
| After-6 months | 1.00 ±0.27 | 2.43 ±0.97 | 3.62 ±1.28 | |||||
| MD (change) | 3.33 | 2.10 | 1.38 | 5.76 | 4.67 | 2.43 | ||
| Improvement % | 49.26% | 29.58% | 22.81% | 85.21% | 65.77% | 40.17% | ||
| P-value | 0.0001* | 0.0001* | 0.0001* | 0.0001* | 0.0001* | 0.0001* | ||
| Plantar fascia thickness | pre-treatment | 0.70 ±0.11 | 0.63 ±0.20 | 0.62 ±0.14 | 0.70 ±0.11 | 0.63 ±0.20 | 0.62 ±0.14 | |
| After-1 month | 0.51 ±0.11 | 0.55 ±0.19 | 0.60 ±0.13 | |||||
| After-6 months | 0.49 ±0.08 | 0.54 ±0.19 | 0.58 ±0.13 | |||||
| MD (change) | 0.19 | 0.08 | 0.02 | 0.21 | 0.09 | 0.04 | ||
| Improvement % | 27.14% | 12.70% | 3.23% | 30.00% | 14.29% | 6.45% | ||
| P-value | 0.0001* | 0.001* | 0.001* | 0.0001* | 0.001* | 0.001* | ||
| Data are expressed as mean ± standard deviation (SD); MD: Mean difference; P-value: probability value; * Significant (P<0.05). | ||||||||
Pairwise comparisons between pre-treatment versus after-1 month as well as before-treatment versus after-6 months before treatment versus after-1 month for pain severity are presented in (Table 3). Time effect had significantly (P<0.05) decreased pain severity after-1 month and after-6 months as compared to pre-treatment within the shockwave group (P=0.0001 & P=0.0001, respectively), phonophoresis group (P=0.0001 & P=0.0001, respectively), and splint group (P=0.0001 & P=0.0001, respectively). The shockwave therapy + conventional program improved higher pain severity after 1-month and after- 6months (49.26 and 85.21%, respectively) than the phonophoresis therapy + traditional program (29.58 and 65.77%, respectively) and splint (conventional) program (22.81 and 40.17%, respectively).
Pairwise comparisons between before-treatment versus after-1 month and before-treatment versus after-6 months before-treatment versus after-1 month for plantar fascia thickness are illustrated in (Table 3). The plantar fascia thickness was significantly (P<0.05) lower after- 1 month and after- 6 months than before treatment in the shockwave group (P=0.0001 & P=0.0001, respectively), phonophoresis group (P=0.001 and P=0.001, respectively), and splint group (P=0.001 & P=0.001, respectively). Improvement percentages for plantar fascia thickness higher in chronic plantar fasciitis patients managed with a shockwave therapy program (27.14 and 30.00, respectively) than phonophoresis therapy program (12.70 and 14.29, respectively) and splint program (3.23 and 6.45%, respectively). These substantial reductions in pain severity, as well as plantar fascia thickness after-1month and after-6 months due to time effect, are more favorable of the shockwave therapy program than the phonophoresis therapy program and splint program (Table 3).
Discussion
The combination of effective therapies may give patients having chronic plantar fasciitis (PF) a new way to improve their symptoms. The goal of this research was to compare and evaluate the long-term impacts of RSWT as well as phonophoresis on patients with chronic PF, as well as to see if there was a link between the change in thickness,
Heel pain is a common symptom of plantar fasciitis (PF). PF is treated with a variety of non-invasive methods. These methods encompass a range of approaches such as steroid injections, NSAIDs, iontophoresis, laser therapy, US therapy, ESWT, orthotic support therapy, as well as exercise-based treatments.(D'Andréa Greve et al., 2009) (Tsai et al., 2010) (Duymaz & Sındel, 2019)(Crawford & Thomson, 2010)(Stuber & Kristmanson, 2006) (Riel et al., 2018), There is disagreement regarding what constitutes the most effective treatment. For this reason, our research is novel, so we designed it to evaluate the synergistic impacts of r-SWT and phonophoresis therapy when added to conventional treatment for PF.
Effects on Pain
Patients with PF often report severe pain as their primary symptom. The first step out of bed usually brings on incredible pain in the medial calcaneal tubercle, which subsides after a few steps but returns in full force after prolonged activity or just before bedtime (Lee et al., 2012), Our research showed that across all three treatment groups, pain was reduced The shockwave therapy + conventional program improved higher pain severity after 1-month and after- 6months (49.26 and 85.21%, respectively) than phonophoresis therapy + traditional program (29.58 and 65.77%, respectively) and splint (conventional) program (22.81 and 40.17%, respectively). We found that all three forms of therapy successfully reduced pain, but that shockwave was particularly beneficial in reducing the pain associated with increased activity. There was no research discovered that compared the efficacy of r-ESWT and phonophoresis in treating pain; however, studies on the effectiveness of ESWT, phonophoresis, as well as conventional therapeutic applications for treating pain all indicated positive results (Bolívar et al., 2013) (Ryan et al., 2014) (Akinoğlu & Köse, 2018) (Vahdatpour et al., 2012) Moreover, these findings corroborated those of our research.
Effects on plantar fascia thickness
The thickness of the plantar fascia was another variable we measured. The diagnostic appearance of plantar fasciitis on Ultrasonography and magnetic resonance imaging has been discussed by several researchers [(Berkowitz et al., 1991), (Draghi et al., 2017) (Ahn et al., 2016), (Ulusoy et al., 2017b) (Romero-Morales et al., 2019). Afflicted sides consistently had thicker tissue than their non-affected counterparts for the plantar fascia. Our research involved the systematic use of ultrasonographic measurements taken one month and six months after applying three therapies. Patients' plantar fascia thickness decreased after treatment began compared to their pre-treatment thickness. Improvement percentages for plantar fascia thickness were higher in chronic PF patients managed with shockwave therapy program (27.14 and 30.00, respectively) than phonophoresis therapy program (12.70 and 14.29, respectively) and splint program (3.23 and 6.45%, respectively). This was thought to be due to the plantar fascia's inherent pliability and elasticity, causing inflammation to subside and the fascia to stretch.
Furthermore, the search of the literature revealed no studies contrasting the impacts of r-ESWT as well as phonophoresis therapies on plantar fascia thickness; however, in the literature (Fabrikant & Park, 2011) measured the plantar fascia thickness before as well as following treatment, and discovered no correlation between a decrease in thickness as well as clinical improvement. Nevertheless, (Mahowald et al., 2011) identified a correlation between the decline in facial thickness (0.82 ± 1.04 mm) as well as increases in pain VAS scores (3.64 ± 2.7). In the current investigation, we found similar results, demonstrating a correlation between fascial thickness decline and pain relief, confirming their previous work. Those who showed the greatest improvement in their function following treatment also had the greatest reduction in fascial thickness. These findings further support using ultrasonographic variations in plantar fascia thickness as a meaningful objective indicator of therapy efficacy.
Functional Outcomes
Regardless of the treatment options undertaken, there are a wide range of different measures of pain and function that have been reported in the literature for patients with additional foot & ankle problems last parameter was the lower extremity functional scale, one of the validated self-report questionnaires used for pre and post-intervention evaluations of treatments for heel pain/plantar fasciitis-related physical impairments, activity limitations, as well as participation restrictions (R. L. Martin et al., 2014b) Since the research employed different scales. We were unable to compare the results. Our study confirms what has been found elsewhere in the literature. Patients experiencing heel pain whose conditions were followed for 1 and 6 months found that treatment procedures had helped them function better. The shockwave group progressed more quickly in their recovery (76.04 and 93.25%, respectively) followed by patients treated by phonophoresis therapy + conventional program (40.35 and 81.47, respectively%) and then those who received splint (traditional) program (26.09 and 47.79%, respectively). (Al-Siyabi et al., 2022) Their outcomes revealed that radial ESWT and US are effective in lessening pain and increasing mobility, but radial ESWT was substantially more effective than the US. (Ulusoy et al., 2017a) Their study involved assessing the clinical outcomes after the treatment period. The three techniques showed improvements in pain VAS scores, heel sensitivity (heel tenderness index), Roles-Maudsley score (activity limitations), and the ankle-hind-foot scale of the AOFAS scale. However, ESWT and laser therapy showed considerably better pain relief and functional outcomes than ultrasound therapy during the onemonth follow-up. There was no substantial difference when comparing the efficacy of laser therapy and ESWT.
These studies show that radial shockwave therapy may be a more effective long-term treatment option for chronic plantar fasciitis than phonophoresis. However, it is critical to remember that every patient has individual requirements and preferences that should be considered before settling on a course of therapy.
It is also crucial to be aware of these treatments' possible hazards and side effects. While radial shockwave therapy and phonophoresis are generally safe and well-tolerated, they may cause pain or discomfort during treatment, and there is a small risk of more serious side effects, such as bruising, swelling, or infection.
In conclusion, the available evidence suggests that radial shockwave therapy may be a more effective long-term treatment option for chronic plantar fasciitis than phonophoresis. It is important to consider the patient's unique circumstances and preferences when making a treatment decision, although more study is needed to corroborate these findings.
Conclusion
Within the limitation of the current research, it could be concluded that: Adding RSWT or phonophoresis to night splints are effective therapeutic modalities in enhancement of pain reduction, plantar fascia thickness, and the improvement of the functionality of the lower extremity at the short-term follow-up one month (4 weeks) and long-termed follow-up six months in the treatment of patients having chronic plantar fasciitis. Although both groups demonstrated improvement, the shockwave group was more noticeable than the phonophoresis group's (p<0,0001).
References
Abul, K., Ozer, D., Sakizlioglu, S. S., Buyuk, A. F., & Kaygusuz, M. A. (2015). Detection of normal plantar fascia thickness in adults via the ultrasonographic method. Journal of the American Podiatric Medical Association, 105(1), 8–13. https://doi.org/10.7547/8750-7315-105.1.8
Ahn, J. H., Lee, C. W., Park, C. J., & Kim, Y. C. (2016). Ultrasonographic examination of plantar fasciitis: A comparison of patient positions during examination. Journal of Foot and Ankle Research, 9(1). https://doi.org/10.1186/s13047-016-0171-4
Akinoğlu, B., & Köse, N. (2018). A comparison of the acute effects of radial extracorporeal shockwave therapy, ultrasound therapy, and exercise therapy in plantar fasciitis. In Journal of Exercise Rehabilitation (Vol. 14, Issue 2, pp. 306–312). https://doi.org/10.12965/jer.1836048.024
Al-Siyabi, Z., Karam, M., Al-Hajri, E., Alsaif, A., Alazemi, M., & Aldubaikhi, A. A. (2022). Extracorporeal Shockwave Therapy Versus Ultrasound Therapy for Plantar Fasciitis: A Systematic Review and Meta-Analysis. Cureus, 14(1), e20871. https://doi.org/10.7759/cureus.20871
Alnahdi, A. H., Alrashid, G. I., Alkhaldi, H. A., & Aldali, A. Z. (2016). Cross-cultural adaptation, validity and reliability of the Arabic version of the Lower Extremity Functional Scale. Disability and Rehabilitation, 38(9), 897–904. https://doi.org/10.3109/09638288.2015.1066452
Bélanger, A., & Bélanger, A. (2010). Therapeutic electrophysical agents : evidence behind practice. Wolters Kluwer Health/Lippincott Williams & Wilkins.
Berkowitz, J. F., Kier, R., & Rudicel, S. (1991). Plantar fasciitis: MR imaging. Https://Doi.Org/10.1148/Radiology.179.3.2027971, 179(3), 665–667. https://doi.org/10.1148/RADIOLOGY.179.3.2027971
Bolívar, Y. A., Munuera, P. V., & Padillo, J. P. (2013). Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot and Ankle International, 34(1), 42–48. https://doi.org/10.1177/1071100712459173
Chuckpaiwong, B., Berkson, E. M., & Theodore, G. H. (2009). Extracorporeal Shock Wave for Chronic Proximal Plantar Fasciitis: 225 Patients with Results and Outcome Predictors. Journal of Foot and Ankle Surgery, 48(2), 148–155. https://doi.org/10.1053/j.jfas.2008.11.001
Crawford, F., & Thomson, C. E. (2010). WITHDRAWN. Interventions for treating plantar heel pain. The Cochrane Database of Systematic Reviews, 1, CD000416. https://doi.org/10.1002/14651858.CD000416.pub2
D’Andréa Greve, J. M., Grecco, M. V., & Santos-Silva, P. R. (2009). Comparison of radial shockwaves and conventional physiotherapy for treating plantar fasciitis. Clinics (Sao Paulo, Brazil), 64(2), 97–103. https://doi.org/10.1590/S1807-59322009000200006
Dedes, V., Tzirogiannis, K., Polikandrioti, M., Dede, A. M., Nikolaidis, C., Mitseas, A., & Panoutsopoulos, G. I. (2019). Radial extracorporeal shockwave therapy versus ultrasound therapy in the treatment of plantar fasciitis. Acta Informatica Medica, 27(1), 45–49. https://doi.org/10.5455/aim.2019.27.45-49
Draghi, F., Gitto, S., Bortolotto, C., Draghi, A. G., & Ori Belometti, G. (2017). Imaging of plantar fascia disorders: findings on plain radiography, Ultrasound, and magnetic resonance imaging. Insights into Imaging, 8(1), 69–78. https://doi.org/10.1007/S13244-016-0533-2/TABLES/1
Duymaz, T., & Sındel, D. (2019). Comparison of Radial Extracorporeal Shock Wave Therapy and Traditional Physiotherapy in Rotator Cuff Calcific Tendinitis Treatment. Archives of Rheumatology, 34(3), 281–287. https://doi.org/10.5606/ARCHRHEUMATOL.2019.7081
Fabrikant, J. M., & Park, T. S. (2011). Plantar fasciitis (fasciosis) treatment outcome study: Plantar fascia thickness measured by Ultrasound and correlated with patient self-reported improvement. The Foot, 21(2), 79–83. https://doi.org/10.1016/J.FOOT.2011.01.015
Gollwitzer, H., Gloeck, T., Roessner, M., Langer, R., Horn, C., Gerdesmeyer, L., & Diehl, P. (2013). Radial Extracorporeal Shock Wave Therapy (rESWT) Induces New Bone Formation in vivo: Results of an Animal Study in Rabbits. Ultrasound in Medicine and Biology, 39(1), 126–133. https://doi.org/10.1016/j.ultrasmedbio.2012.08.026
Gonnade, N., Bajpayee, A., Elhence, A., Lokhande, V., Mehta, N., Mishra, M., & Kaur, A. (2018). Regenerative efficacy of therapeutic quality platelet-rich plasma injections versus phonophoresis with kinesiotaping for the treatment of chronic plantar fasciitis: A prospective randomized pilot study. Asian Journal of Transfusion Science, 12(2), 105–111. https://doi.org/10.4103/ajts.AJTS_48_17
Grecco, M. V., Brech, G. C., & Greve, J. M. D. A. (2013). One-year treatment follow-up of plantar fasciitis: radial shockwaves vs. conventional physiotherapy. Clinics, 68(8), 1089. https://doi.org/10.6061/CLINICS/2013(08)05
Hossain, M., & Makwana, N. (2011). "Not Plantar Fasciitis": The differential diagnosis and management of heel pain syndrome. Orthopaedics and Trauma, 25(3), 198–206. https://doi.org/10.1016/j.mporth.2011.02.003
Johns, L. D. (2002). Non-thermal Effects of Therapeutic Ultrasound: The Frequency Resonance Hypothesis. Journal of Athletic Training, 37(3), 293. /pmc/articles/PMC164359/
Johnson, R. E., Haas, K., Lindow, K., & Shields, R. (2014). Plantar fasciitis: What is the diagnosis and treatment? Orthopaedic Nursing, 33(4), 198–204. https://doi.org/10.1097/NOR.0000000000000063
Laurent, D., & Leung, Y. Y. (2006). Measurement of pain using the visual numeric scale Cite this paper Related papers T he Sout h Aust ralia Healt h Chronic Disease Self-Management Int ernet Trial. http://patienteducation.stanford.edu/research/vnspain.pdf.
Lee, W. C. C., Wong, W. Y., Kung, E., & Leung, A. K. L. (2012). Effectiveness of adjustable dorsiflexion night splint in combination with accommodative foot orthosis on plantar fasciitis. Journal of Rehabilitation Research and Development, 49(10), 1557–1564. https://doi.org/10.1682/JRRD.2011.09.0181
Loske, A. M. (2017). Medical and Biomedical Applications of Shock Waves. In Medical and Biomedical Applications of Shock Waves (pp. 189–250).
Mahowald, S., Legge, B. S., & Grady, J. F. (2011). The Correlation Between Plantar Fascia Thickness and Symptoms of Plantar Fasciitis. Journal of the American Podiatric Medical Association, 101(5), 385–389. https://doi.org/10.7547/1010385
Martin, J. E., Hosch, J. C., Preston Goforth, W., Murff, R. T., Matt Lynch, D., & Odom, R. D. (2001). Mechanical Treatment of Plantar Fasciitis: A Prospective Study. Journal of the American Podiatric Medical Association, 91(2), 55–62. https://doi.org/10.7547/87507315-91-2-55
Martin, R. L., Davenport, T. E., Reischl, S. F., McPoil, T. G., Matheson, J. W., Wukich, D. K., McDonough, C. M., Altman, R. D., Beattie, P., Cornwall, M., Davis, I., DeWitt, J., Elliott, J., Irrgang, J. J., Kaplan, S., Paulseth, S., Torburn, L., Zachazewski, J., & Godges, J. J. (2014a). Heel pain - Plantar fasciitis: Revision 2014. Journal of Orthopaedic and Sports Physical Therapy, 44(11), A1–A33. https://doi.org/10.2519/JOSPT.2014.0303
Martin, R. L., Davenport, T. E., Reischl, S. F., McPoil, T. G., Matheson, J. W., Wukich, D. K., McDonough, C. M., Altman, R. D., Beattie, P., Cornwall, M., Davis, I., DeWitt, J., Elliott, J., Irrgang, J. J., Kaplan, S., Paulseth, S., Torburn, L., Zachazewski, J., & Godges, J. J. (2014b). Heel pain - Plantar fasciitis: Revision 2014. In Journal of Orthopaedic and Sports Physical Therapy (Vol. 44, Issue 11, pp. A1–A33). Movement Science Media. https://doi.org/10.2519/jospt.2014.0303
Moher, D., Schulz, K. F., Altman, D. G., & Lepage, L. (2001). The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Medical Research Methodology, 1, 2. https://doi.org/10.1186/1471-2288-1-2
Morrissey, D., Cotchett, M., Said J'bari, A., Prior, T., Griffiths, I. B., Rathleff, M. S., Gulle, H., Vicenzino, B., & Barton, C. J. (2021). Management of plantar heel pain: A best practice guide informed by a systematic review, expert clinical reasoning and patient values. In British Journal of Sports Medicine (Vol. 55, Issue 19, pp. 1106–1118). https://doi.org/10.1136/bjsports-2019-101970
Owens, B. D., Wolf, J. M., Seelig, A. D., Jacobson, I. G., Boyko, E. J., Smith, B., Ryan, M. A. K., Gackstetter, G. D., & Smith, T. C. (2013). Risk factors for lower extremity tendinopathies in military personnel. Orthopaedic Journal of Sports Medicine, 1(1), 1–8. https://doi.org/10.1177/2325967113492707
Riel, H., Vicenzino, B., Jensen, M. B., Olesen, J. L., Holden, S., & Rathleff, M. S. (2018). The effect of isometric exercise on pain in individuals with plantar fasciopathy: A randomized crossover trial. Scandinavian Journal of Medicine & Science in Sports, 28(12), 2643–2650. https://doi.org/10.1111/SMS.13296
Romero-Morales, C., Martín-Llantino, P. J., Calvo-Lobo, C., López-López, D., Sánchez-Gómez, R., De-La-Cruz-Torres, B., & Rodríguez-Sanz, D. (2019). Ultrasonography Features of the Plantar Fascia Complex in Patients with Chronic Non-Insertional Achilles Tendinopathy: A Case-Control Study. Sensors (Basel, Switzerland), 19(9). https://doi.org/10.3390/S19092052
Ryan, M., Hartwell, J., Fraser, S., Newsham-West, R., & Taunton, J. (2014). Comparison of a physiotherapy program versus dexamethasone injections for plantar fasciopathy in prolonged standing workers: A randomized clinical trial. Clinical Journal of Sport Medicine, 24(3), 211–217. https://doi.org/10.1097/JSM.0000000000000021
Silbernagel, K. G., Hanlon, S., & Sprague, A. (2020). Current Clinical Concepts: Conservative Management of Achilles Tendinopathy. Journal of Athletic Training, 55(5), 438. https://doi.org/10.4085/1062-6050-356-19
Simplicio, C. L., Purita, J., Murrell, W., Santos, G. S., dos Santos, R. G., & Lana, J. F. S. D. (2020). Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. Journal of Clinical Orthopaedics and Trauma, 11(Suppl 3), S309. https://doi.org/10.1016/J.JCOT.2020.02.004
Stuber, K., & Kristmanson, K. (2006). Conservative therapy for plantar fasciitis: a narrative review of randomized controlled trials. The Journal of the Canadian Chiropractic Association, 50(2), 118. /pmc/articles/PMC1839987/
Thomas, M. J., Whittle, R., Menz, H. B., Rathod-Mistry, T., Marshall, M., & Roddy, E. (2019). Plantar heel pain in middle-aged and older adults: Population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC Musculoskeletal Disorders, 20(1). https://doi.org/10.1186/s12891-019-2718-6
Thompson, J. V., Saini, S. S., Reb, C. W., & Daniel, J. N. (2014). Diagnosis and management of plantar fasciitis. In Journal of the American Osteopathic Association (Vol. 114, Issue 12, pp. 900–906). American Osteopathic Association. https://doi.org/10.7556/jaoa.2014.177
Tsai, C. T., Chang, W. D., & Lee, J. P. (2010). Effects of Short-term Treatment with Kinesiotaping for Plantar Fasciitis. Http://Dx.Doi.Org/10.3109/10582450903495882, 18(1), 71–80. https://doi.org/10.3109/10582450903495882
Ulusoy, A., Cerrahoglu, L., & Orguc, S. (2017a). Magnetic Resonance Imaging and Clinical Outcomes of Laser Therapy, Ultrasound Therapy, and Extracorporeal Shock Wave Therapy for Treatment of Plantar Fasciitis: A Randomized Controlled Trial. In Journal of Foot and Ankle Surgery (Vol. 56, Issue 4, pp. 762–767). https://doi.org/10.1053/j.jfas.2017.02.013
Ulusoy, A., Cerrahoglu, L., & Orguc, S. (2017b). Magnetic Resonance Imaging and Clinical Outcomes of Laser Therapy, Ultrasound Therapy, and Extracorporeal Shock Wave Therapy for Treatment of Plantar Fasciitis: A Randomized Controlled Trial. The Journal of Foot and Ankle Surgery : Official Publication of the American College of Foot and Ankle Surgeons, 56(4), 762–767. https://doi.org/10.1053/J.JFAS.2017.02.013
Vahdatpour, B., Sajadieh, S., Bateni, V., Karami, M., & Sajjadieh, H. (2012). Extracorporeal shock wave therapy in patients with plantar fasciitis. A randomized, placebo-controlled trial with ultrasonographic and subjective outcome assessments. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, 17(9), 834. /pmc/articles/PMC3697207/.