Research Article - (2024) Volume 19, Issue 6
NON-ADHERENCE TO DIABETES MEDICATION WITH RECURRING DIABETIC KETOACIDOSIS AND SUBSEQUENT DEPRESSION: A SYSTEMATIC REVIEW
Abdelrahman Mohamed Ahmed Abukanna1*, Ahmed Hamad Ahmed Sulaiman2, Mathayil Nazal Alruwaili3, Ashwaq Ibrahim H Alanazi4, Hala Abdullah Alanazi4, Miad Daham R Alanazi5, Nawaf Abdulaziz Almudiheem6, Maram Saleh AL Ruwaili7, Sarah Abdulqader Albalawi8, Kholoud Ali Althobaiti9, Amal Saeed Alzaidi10 and Ola Mayouf Alsufyani11*Correspondence: Abdelrahman Mohamed Ahmed Abukanna, Associate Professor of Internal Medicine, Faculty of Medicine, Northern Border University, Saudi Arabia, Email:
2Assistant Professor, Department of Internal Medicine, Faculty of Medicine, Northern Border University, Arar, Saudi Arabia
3General Practitioner, Department of Internal Medical, King Abdulaziz Hospital, Aljouf Region, Saudi Arabia
4Intern, Faculty of Medicine, Northern Border University, Saudi Arabia
5Nursing Specialist, Maternity And Children Hospital, Arar, Saudi Arabia
6General Directory, Prison Health, Riyadh, Saudi Arabia
7Emergency Nursing Specialist, Maternity and Children Hospital, Aljouf Health Cluster, Aljouf, Saudi Arabia
8Pharm D Program, Faculty of Pharmacy, University of Tabuk, Saudi Arabia
9Finished internship, Faculty of Pharmacy, Taif University, Saudi Arabia
10Pharmacists Volunteer, Pharmacy Department, Armed Forces Center for Rehabilitation, Taif, Saudi Arabia
11Intern, Faculty of Pharmacy, Taif University, Saudi Arabia
Received: 01-Dec-2024 Published: 15-Dec-2024
Abstract
Objectives: To systematically evaluate and synthesize existing evidence on the association between depression and the risk of readmission or recurrence of diabetic ketoacidosis (DKA).
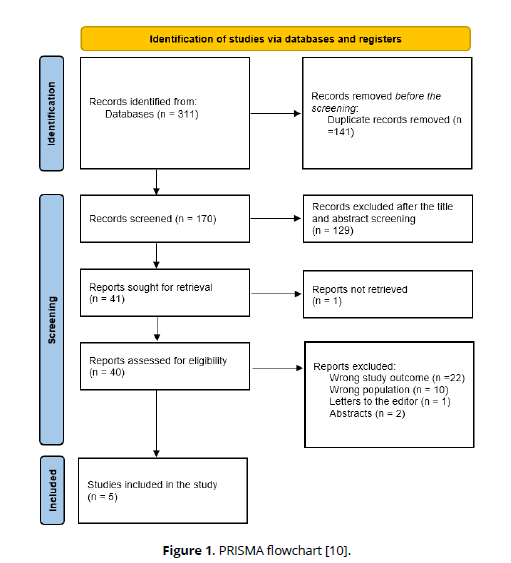
Methods: A comprehensive search across four databases identified 311 publications. Duplicates were removed using Rayyan QCRI, and relevance screening reduced the selection to 40 full-text articles. After further review, five studies met the inclusion criteria.
Results: Five studies involving 615,502 participants were analyzed, with females making up 48.7% of the population. Two studies reported depression prevalence among patients with DKA, showing rates of 12.3% and 46.3%. Recurrence rates were notably high, reaching 55.4% and 50%, while readmission rates varied between 4.7% and 12.3%. Studies show a strong connection between depression and DKA readmission. Patients with depression, especially those with psychosis, are at higher risk for general and 30-day readmission. While depression is more frequent in recurrent DKA cases, its severity does not differ between single and multiple episodes. This association remains consistent over time. However, one casecontrol study found no significant difference in depression symptoms between cases and controls, indicating variability and the need for further investigation.
Conclusion: This is the first systematic review to examine the link between depression and DKA readmission or recurrence, highlighting the critical role of mental health in diabetes outcomes. Integrating depression screening and management into diabetes care may help reduce DKA episodes and improve patient outcomes. The findings support the need for enhanced mental health services as part of diabetes management. Future research should focus on longitudinal studies and standardized depression assessments to clarify this relationship and develop more effective interventions to reduce recurrent DKA.
Keywords
Diabetes mellitus. Diabetic ketoacidosis. Recurrence. Readmission. Depression. Psychological assessment. Systematic review
Introduction
A potentially fatal consequence of diabetes, DKA is characterized by a metabolic acidosis brought on by hyperketonaemia [1]. Beta-hydroxybutyrate, acetoacetate, and acetone are examples of ketones, which are breakdown products of fatty acids [2]. Although fasting can result in ketoacidosis, diabetes patients are more likely to experience it because of insulin deficiency and insulin-mediated glucose absorption into cells [3]. As a result, there is insufficient intracellular glucose, which causes fat to be broken down for energy [1].
DKA can be brought on by physiological stressors or occurs when diabetes is not adequately managed [1]. Although the rate of DKA hospitalizations rose 6.3% between 2009 and 2014, hospital case-fatality decreased from 1.1% to 0.04 percent during the same period due to improved protocols and treatment [4].
Due to inadequate glucose monitoring, patients with psychiatric illnesses are more likely to develop DKA [5]. DKA is more likely to occur in patients with type 1 diabetes and depression [6, 7]. There might be more nuance to this association, too, as a recent study by Garrett et al. revealed a strong correlation between attachment issues and inadequate diabetes management that leads to recurrent DKA episodes [8].
DKA is one of the serious diabetic complications that has repeated incidence, leading to the increased burden of healthcare and morbidity in patients. Emerging evidence shows that, among individuals with diabetes, psychological conditions, especially depression, is associated with poor management of treatment, hence increasing vulnerability in DKA patients for its recurrence. However, the association between depression and readmission to DKA is not well described, which thus provides a rationale for performing a systematic review and meta-analysis that can synthesize evidence on this association. The results may help in formulating interventions that can decrease readmission rates and improve outcomes among these patients.
The aim of this review is to systematically evaluate and synthesize existing evidence on the association between depression and the risk of readmission or recurrence of DKA, with the goal of identifying patterns, assessing the strength of the relationship, and guiding future research and clinical practice.
Methods
Search strategy
The PRISMA and GATHER criteria were followed for the systematic review. An overall search was conducted to identify relevant studies related to the association between depression and the risk of readmission or recurrence of DKA. The following four electronic databases were used by the reviewers for searching: SCOPUS, Web of Science, Cochrane, and PubMed. We removed any duplicates and uploaded all the titles and abstracts we could find through electronic searches onto Rayyan. After that, all the study texts that met the inclusion criteria based on the abstract or title were collected for a full-text examination. Two reviewers independently evaluated the extracted papers' suitability and discussed any discrepancies.
Study population-selection
The PEO (Population, Exposure, and Outcome) factors were implemented as inclusion criteria for our review: (i) Population: Patients with diabetes who have experienced DKA, (ii) Exposure: Presence of depression (diagnosed or self-reported), (iii) Outcome: Readmission or recurrence of DKA.
Data extraction
Data from studies that satisfied the inclusion requirements were extracted by two objective reviewers using a predetermined and uniform methodology. The following information was retrieved and recorded: (i) First author (ii) Year of publication, (iii) Study design, (iv) Country, (v) Sample size, (vi) Age, (vii) Gender, (viii) Diagnostic tool of depression, (ix) Concurrent event, (x) Incidence of depression (%), (xi) Incidence of readmission/ recurrence (xii) Main outcomes.
Quality review
Since bias resulting from omitted factors is frequent in studies in this field, we used the ROBINS-I technique to assess the likelihood of bias since it enables a thorough examination of confounding. The ROBINS-I tool can be used for cohort designs where individuals exposed to different staffing levels are tracked over time and is designed to assess non-randomized studies. Each paper's risk of bias was evaluated independently by two reviewers, and any differences were settled by group discussion [9].
Results
The specified search strategy yielded 311 publications (Figure 1). After removing duplicates (n = 141), 170 trials were evaluated based on title and abstract. Of these, 129 failed to satisfy eligibility criteria, leaving just 38 full-text articles for comprehensive review. A total of 5 satisfied the requirements for eligibility with evidence synthesis for analysis (Figure 1).
Sociodemographic and clinical outcomes
We included five studies with a total of 615,502 participants and the majority 299,929 (48.7%) were females. Regarding study designs, three were retrospective cohorts [11, 12, 14], one was a cross-sectional study [13], and one was a case-control study [10, 11, 13, 14]. Three studies were implemented in the USA [12-14], one in Peru [11], and one in the UK [15]. The earliest study was conducted in 2011 [13] and the latest in 2021 [14, 15].
Two studies reported the prevalence of depression among patients with DKA (12.3%) [11] and 46.3% [13], while the other studies included odds ratios for the incidence of depression. The incidence of recurrence was high 55.4% [13] and 50% [15], while the incidence of readmission ranged from 4.7% [12] to 12.3% [11]. One study indicated the prevalence of depression was significantly higher among patients readmitted within thirty days compared to their non-readmitted counterparts; thus, there is a strong association between mental health and short-term returns to the hospital [11]. Another paper also points out that the presence of major depression with psychosis increases the risk of general and 30-day readmission for DKA, proving that psychiatric comorbidities can worsen the chances of recurrence [12].
Whereas, in one cohort, a history of depression was more probable among patients experiencing recurrent DKA. However, the severity of depression was similar in the group with multiple episodes as compared to the group with a single episode, with PHQ-9 scores showing that though depression is high, its intensity may not relate directly to the frequency of DKA [13]. Another analysis supporting the temporal consistency in the association of depression with higher DKA readmission extends the belief of the sustained effect of psychiatric factors on diabetic outcome [14].
On the other hand, a case-control study performed shows that symptoms of depression were not significantly different between cases and controls by adjusted multiple-test analysis [15] (Table 1, Table 2).
| Study ID | Study design | Country | Sociodemographic | AKI incidence (%) | Concurrent event | Depression (%) | Readmission/ recurrence (%) | Main outcomes |
|---|---|---|---|---|---|---|---|---|
| Hurtado et al., 2019 [11] | Retrospective cohort | Peru | N= 479,590 Mean age: 42.4 Males: 228,525 (47.7%) |
Retrospective hospital records | Readmission | 59,085 (12.3%) | 58,961 (12.3%) | Patients who were re-admitted within thirty days had a higher prevalence of depression, with more cases observed compared to those who were not re-admitted. |
| Bhatt et al., 2020 [12] | Retrospective cohort | USA | N= 116,183 Age range: 2-18 Males: 61,460 (52.9%) |
Retrospective hospital records | Readmission | NM | 5427 (4.7%) | Patients with depression and psychosis had higher risks of readmission and 30-day readmission due to DKA alone. |
| Randall et al., 2011 [13] | Cross-sectional | USA | N= 164 Mean age: 40.8 |
PHQ-9 | Recurrence | 76 (46.3%) | 91 (55.5%) | Patients with recurrent DKA admissions had a higher history of depression; however, PHQ-9 scores did not differ between patients with many episodes and those with a single episode. |
| Males: 106 (64.6%) | ||||||||
| Vasireddy et al., 2021 [14] | Retrospective cohort | USA | N= 19,519 | Retrospective hospital records | Readmission | NM | 831 (8.5%) | This study observed a tendency that has remained constant over time: those with depression also had increased risks of a 30-day DKA readmission. |
| Garrett et al., 2021 [15] | Case-control | UK | Age range: 0-18 Males: 9822 (50.3%) N= 46 Mean age: 31 Males: 16 (34.8%) |
BDI-II | Recurrence | NM | 23 (50%) | After controlling for multiple testing, there was no discernible difference in depression symptoms between cases and controls. |
| Study ID | Bias due to confounding | Bias in the selection of participants into | Bias in the classification of interventions | Bias due to deviations from the intended interval | Bias due to missing data | Bias in the measurement of outcomes | Bias in the selection of reported result | Overall bias |
|---|---|---|---|---|---|---|---|---|
| Hurtado et al., 2019 [11] | Mod | Mod | Low | Low | Low | Low | Low | Low |
| Bhatt et al., 2020 [12] | Low | Mod | Low | Low | Low | Mod | Low | Low |
| Randall et al., 2011 [13] | Low | Low | Low | Low | Low | Low | Mod | Low |
| Vasireddy et al., 2021 [14] | Mod | Mod | Low | Low | Low | Mod | Mod | Moderate |
| Garrett et al., 2021 [15] | Mod | Mod | Low | Low | Low | Mod | Mod | Moderate |
Discussion
This is the first systematic review to explore the association between depression and the risk of DKA readmission or recurrence. This systematic review provides an overview of main results: there is a strong association of depression with readmission or recurrence of DKA. In all, patients with major depression consistently showed higher rates of readmission, especially with psychosis, thus showing that mental health issues may lead to poor diabetes management. This association indicates a bidirectional influence of the mind and body, where an untreated psychiatric illness can worsen the course of a physical illness, and vice versa. According to a comprehensive analysis by Pompili et al., young males with type 1 diabetes have a significant suicide rate, peaking between the ages of 15 and 29. Given the connection between suicidal thoughts and treatment compliance, they suggested that doctors regularly inquire about suicidal thoughts from their young patients [16]. Adolescents with diabetes are more likely to experience mental health disorders, noncompliance with their treatment plans, and suicide ideation. It has been discovered that adolescents with a lifetime history of suicide thoughts are more likely to not follow their prescribed treatment plan [17].
Some research suggests that depression and diabetes may share inflammatory pathways, and it is possible that similar mechanisms underlie the link between each condition's severe syndrome [18]. Co-morbid mood and other mental disorders can be treated in conjunction with diabetes management, as there is some potential in using mental health treatments for individuals with recurrent DKA [19].
It is crucial to take into account the significant influence of socioeconomic factors related to education, housing, and unemployment as factors to the development of DKA, in addition to the potential for depression and/or diabetes distress. In the current study, DKA was linked to a number of detrimental social characteristics, such as lower levels of formal education, increased unemployment, and illegal drug usage. It is well recognized that these elements contribute to the onset of depression and in turn [20].
This field is complicated. Depression, "diabetes burnout," and the negative socioeconomic variables of unemployment, low educational attainment, unstable housing, and insufficient financial resources often interact in both directions. It's also probable that the stress of caring for diabetes, rather than severe depressive illness in general, was a major contributing factor to the suffering [21]. However, we are unable to respond to these crucial questions due to the current study's narrow scope.
This finding strongly associates depression with DKA recurrence and thus suggests that optimal diabetes care should include screening for and treatment of mental disorders. Routine assessment of depression in all diabetic patients, especially those with a previous history of DKA, may be useful in the early identification of patients who are at an increased risk for readmission. Incorporating psychiatric support and counselling into regular diabetes management plans may help prevent DKA recurrence and thus yield better long-term results. Multidisciplinary approaches have an important role, involving endocrinologists, mental health specialists, and diabetes educators in addition to the healthcare provider. Early intervention for depressive symptoms may help prevent DKA recurrence and generally improve diabetes control and well-being in patients.
Strengths
This review has a strong point in its large sample size and good heterogeneity; hence, it responds well to generalization across populations. The search process was elaborate: it used Rayyan QCRI for duplicate removal and relevance screening to ensure systematic, unbiased study selection. Focusing on both readmission and recurrence, the review therefore gives a more balanced insight into the ways through which depression may influence both the short-term and long-term outcomes of DKA. This has, therefore, enabled a more holistic investigation of the interrelationship between psychiatric and metabolic health.
Limitations
Despite these strengths, there are several limitations to this review. The heterogeneity of design, population characteristics, and methods used for the assessment of depression in the included studies may account for the inconsistencies seen in some results. Moreover, not all studies reported the severity of depression, which limits the ability to assess whether the intensity of depressive symptoms is related to DKA recurrence. Most of the data were from retrospective studies; hence, recall bias may arise, and the reliability of such findings is in question. Besides, there are only five studies that meet the inclusion criteria. The overall sample of studies remains small, and further research is required to strengthen the evidence base.
Conclusion
This systematic review is the first on the association of depression with readmission or recurrence of DKA, emphasizing how important mental health is in diabetes outcomes. Addressing depression should be an integral part of comprehensive diabetes care for reducing the frequency of DKA episodes and improving clinical outcomes. The findings call for increased integration of mental health services into diabetes care, with early detection and management of depression. Further studies are needed to focus more on longitudinal studies and use a more standardized approach to assessing depression; this would help to provide further clarification of the relationship and inform better interventions that aim at a reduction in the burden of recurrent DKA.
References
Virdi N, Poon Y, Abaniel R, Bergenstal RM. Prevalence, cost, and burden of diabetic ketoacidosis. Diabetes Technology & Therapeutics. 2023 Jun 1;25(S3):S-75.
Goldstein DE, Little RR, Lorenz RA, Malone JI, Nathan D, Peterson CM, Sacks DB. Tests of glycemia in diabetes. Diabetes care. 2004 Jul 1;27(7):1761-73.
Barski L, Eshkoli T, Brandstaetter E, Jotkowitz A. Euglycemic diabetic ketoacidosis. European journal of internal medicine. 2019 May 1; 63:9-14.
Benoit SR. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality—United States, 2000–2014. MMWR. Morbidity and mortality weekly report. 2018;67.
5] Garrett C, Doherty A. Diabetes and mental health. Clin Med (Lond) 2014;14(6): 669–72.
McGrady ME, Laffel L, Drotar D, Repaske D, Hood KK. Depressive symptoms and glycemic control in adolescents with type 1 diabetes: mediational role of blood glucose monitoring. Diabetes Care 2009;32(5):804–6.
Trief PM, Xing D, Foster NC, Maahs DM, Kittelsrud JM, Olson BA, et al. Depression in adults in the T1D Exchange Clinic Registry. Diabetes Care 2014;37(6):1563–72.
Garrett CJ, Moulton CD, Choudhary P, Amiel SA, Fonagy P, Ismail K. The psychopathology of recurrent diabetic ketoacidosis: A case-control study. Diabet Med. 2020: e14505.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. bmj. 2016 Oct 12;355.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Prisma-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015 Dec; 4:1-9.
Hurtado CR, Lemor A, Vallejo F, Lopez K, Garcia R, Mathew J, Galindo RJ. Causes and predictors for 30-day re-admissions in adult patients with diabetic ketoacidosis in the United States: a nationwide analysis, 2010–2014. Endocrine Practice. 2019 Mar 1;25(3):242-53.
Bhatt P, Dave M, Amponsah JK, Jain A, Yagnik P, Asare‐Afriyie B, Donda K, Sharma M, Parmar N, Patel A, Bhatt N. Etiologies, trends, and predictors of 30‐day pediatric readmissions after hospitalizations for diabetic ketoacidosis in the United States. Pediatric Diabetes. 2020 Sep;21(6):969-78.
Randall L, Begovic J, Hudson M, Smiley D, Peng L, Pitre N, Umpierrez D, Umpierrez G. Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Diabetes care. 2011 Sep 1;34(9):1891-6.
Vasireddy D, Sehgal M, Amritphale A. Risk factors, trends, and preventive measures for 30-day unplanned diabetic ketoacidosis readmissions in the pediatric population. Cureus. 2021 Nov;13(11).
Garrett CJ, Moulton CD, Choudhary P, Amiel SA, Fonagy P, Ismail K. The psychopathology of recurrent diabetic ketoacidosis: A case–control study. Diabetic Medicine. 2021 Jul;38(7):e14505.
Pompili M., Forte A., Lester D., Erbuto D., Rovedi F., Innamorati M., et al. Suicide risk in type 1 diabetes mellitus: A systematic review. J Psychosom Res. 2014;76(5):352–360.
Pelizza L., Pupo S. Brittle diabetes: Psychopathology and personality. J Diabetes Complications. 2016;30(8):1544–1547.
Moulton C.D., Pickup J.C., Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015 Jun;3(6):461–471.
Garrett C.J., Moulton C.D., Lee T., Amiel S.A., Fonagy P., Ismail K. Can a mental health treatment reduce admissions for diabetic ketoacidosis? Acta Diabetol. 2023 Mar;60(3):455–457.
PHE AC. National Health Priority Areas Report.
Hamblin PS, Abdul‐Wahab AL, Xu SF, Steele CE, Vogrin S. Diabetic ketoacidosis: a canary in the mine for mental health disorders? Internal Medicine Journal. 2022 Jun;52(6):1002-8.