Research Article - (2025) Volume 20, Issue 1
Staffing Levels Work Schedules Required Overtime And Turnover In Acute Care Hospitals Impact Health Care Workers Burnout
ATEF EID MADKOUR ELSAYED1*, AHMED ABDULLAH MOHAMMED ALSHEHRI2, Elaf Alshehri3, Raghad Ayman Sairafi4, Sami khalif alenazi5, Hadeel Abdulrahman Hashem6, Hajer Aiydh Alsalmi7, Ghada Saleh Magnas8, Fahad Saad ALMATHKER9, Mohammed Almaghlouth10, Monther Abdullah Aldossary11 and Farah Tarek Ahmed Mehana12*Correspondence: ATEF EID MADKOUR ELSAYED, Consultant cardiology, King abdelaziz hospital sakaka, Saudi Arabia, Email:
2Radiology Technologist, Almjardah general hospital, Saudi Arabia
3College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
4King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
5Medicine and surgery, Saudi Arabia
6Radiology Technology, Saudi Arabia
7Dentist, Al-halqah phc, Saudi Arabia
8Dental Medicine & Surgery (BDS), Saudi Arabia
9General practice, Saudi Arabia
10Psychiatry, Saudi Arabia
11Oral and maxillofacial surgery, Saudi Arabia
12Medicine and surgery, Saudi Arabia
Received: 03-Feb-2025 Published: 17-Feb-2025
Abstract
Background: Healthcare workers in acute care hospitals face significant challenges related to staffing levels, work schedules, required overtime, and turnover, which contribute to burnout, reduced job satisfaction, and higher turnover intentions. These issues negatively impact both staff well-being and the quality of patient care.
Methods: A cross-sectional study was conducted among 400 healthcare workers in acute care hospitals, including nurses, physicians, and allied health professionals. Data were collected using a structured questionnaire covering staffing levels, work schedules, overtime, burnout (Maslach Burnout Inventory), job satisfaction, and intention to leave. Statistical analyses, including Pearson’s correlation and multiple regression, were employed to assess relationships and predictive effects of key variables.
Results: The study revealed moderate burnout levels (mean MBI score = 38.7, SD = 9.3), with 68% of participants dissatisfied with their jobs and 42% intending to leave within a year. Regression analysis demonstrated that higher patient loads, longer work hours, and required overtime significantly predicted increased burnout (β = 0.45, p < 0.01), decreased job satisfaction (β = -0.42, p < 0.01), and greater turnover intentions (β = 0.32, p < 0.01). Notably, 70% of participants managed more than five patients per shift, and 62% worked over 40 hours per week.
Conclusion: The findings emphasize the urgent need for systemic reforms in acute care hospitals to address inadequate staffing, excessive work hours, and required overtime. Implementing evidence-based strategies to improve staffing practices and promote workforce well-being can enhance job satisfaction, reduce burnout, and improve patient care quality.
Keywords
Healthcare workers, Burnout, Job satisfaction, Staffing levels, Turnover intentions.
Introduction
The management of staff in acute care hospitals is a major issue that challenges all healthcare systems worldwide. The utilization of strict staffing strategies is essential for maintaining the high patient acuity and rapid turnover rates observed in these facilities. The well-being of healthcare workers is at risk due to concerns about staffing levels, work schedules, overtime requirements, and turnover rates (Brook et al., 2019).
Stress and burnout among healthcare workers have long been identified as a result of inadequate staffing levels. Poor nurse-patient ratios often lead to increased workloads and decreased patient time, thereby compromising care. Furthermore, these circumstances cause an atmosphere of elevated stress for medical practitioners, leading to increased frustration and tiredness (World Health Organization, 2020).
Work patterns, particularly those involving irregular or extended work hours, contribute to these difficulties. Circadian rhythms) and rotating shifts and night work make you physically and mentally exhausted. The disruption commonly manifests as reduced job satisfaction and an increased likelihood of care blunders, harming both staff and patients (International Council of Nurses, 2021).
The healthcare team's workforce is also impacted by mandatory or voluntary overtime, which has become increasingly important. While it is a solution to temporary staffing shortages, working excessive hours can lead to chronic fatigue. As they age, this can weaken their ability to provide safe and appropriate care, leading to increased burnout and job dissatisfaction. Additionally (Buchan and Howard, 2022).
Intensive care facilities face additional obstacles due to high turnover rates. The. Health care organizations face a double blow when it comes to recruitment, onboarding, and training costs due to turnover, which also disrupt teamwork. Furthermore, the continuous arrival of new staff can diminish knowledge of institutions and damage working relationships, thereby impacting care quality overall (Nelson-Brantley et al., 2018).
These staffing difficulties often result in burnout, which is characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment. Due to their prolonged exposure and lack of support and resources, healthcare workers are at risk of experiencing this debilitating syndrome. Not only does burnout affect individual workers but also has farreaching effects on health care systems, including lower productivity, higher absenteeism and compromised patient outcomes (Kerzman et al., 2020).
Absent staffing practices are another cause of concern. People who are not satisfied with their work or are under stress may be inclined to consider quitting. Why? This pattern intensifies the problem of staffing shortages, creating a vicious cycle that's hard to break even without systemic actions (Bae et al., 2014).
On the other hand, job satisfaction is a significant safeguard against burnout and turnover. People who feel respected and rewarded tend to maintain their commitment to their jobs.' In acute care settings, job satisfaction is often influenced by factors such as equitable compensation, effective management, and professional development (Bourgon Labelle et al., 2019).
There is a significant interdependence between staffing levels, work schedules, overtime requirements, and turnover patterns, making it imperative to address these issues comprehensively. The development of evidence-based strategies that prioritize employee welfare and patient safety is a crucial task for policymakers, hospital administrators, or healthcare leaders working together (Organization for Economic Co-operation and Development, 2021).
The research examines the intricate connections between these variables and their influence on healthcare workers' burnout, desire to leave, and job satisfaction. These variables are analyzed in this study. It identified key determinants and outcomes that could inform policies and practices on how to improve the quality of care provided to patients in acute care hospitals while also increasing the sustainability of the healthcare workforce.
Methodology
Study Design
This research utilized a cross-sectional study design to examine the relationship between staffing levels, work schedules, required overtime, and turnover and their effects on healthcare workers’ burnout, intention to leave, and job satisfaction in acute care hospitals. The design enabled the collection of data at a single point in time, providing a comprehensive understanding of the interplay between these variables.
Study Setting
The study was conducted in acute care hospitals, focusing on healthcare professionals working in diverse settings such as medical-surgical wards, intensive care units, and emergency departments. These settings were chosen for their high patient acuity and rapid turnover, which are critical factors influencing staff well-being.
Study Population
The study targeted healthcare workers employed in acute care hospitals, including nurses, physicians, and allied health professionals. The inclusion and exclusion criteria ensured the relevance of participants:
1. Inclusion Criteria:
• Full-time employees with at least six months of experience in their current roles.
• Healthcare workers involved directly in patient care.
2. Exclusion Criteria:
• Employees in administrative roles or non-clinical positions.
• Temporary or agency staff.
Sample Size and Sampling Technique
The study included a total of 400 participants, determined based on statistical calculations to ensure sufficient power for detecting associations between variables. A stratified random sampling technique was used to ensure representation from various professional categories (e.g., nurses, physicians) and departments (e.g., intensive care, emergency).
Data Collection Tool
A structured questionnaire was used to collect data from participants. The questionnaire was divided into five sections
1. Demographics: Age, gender, professional role, years of experience, and educational background.
2. Staffing Levels and Work Schedules: Number of patients cared for during a typical shift, average shift duration, and frequency of night or rotating shifts.
3. Overtime and Turnover: Frequency of required overtime, reasons for turnover, and perceived adequacy of staffing.
4. Burnout: Measured using the Maslach Burnout Inventory (MBI), focusing on emotional exhaustion, depersonalization, and personal accomplishment.
5. Job Satisfaction and Intention to Leave: Assessed using validated scales such as the Job Satisfaction Survey (JSS) and a single-item measure for intention to leave.
Data Collection Process
Participants were recruited during staff meetings or via email invitations distributed through hospital administrative offices. The questionnaire was administered electronically using secure survey software to ensure convenience and anonymity. Participation was voluntary, and informed consent was obtained before data collection.
Data Analysis
Data were analyzed using SPSS software (version XX). Descriptive statistics, including means, frequencies, and percentages, were used to summarize demographic characteristics and key variables. Inferential statistics included:
1. Pearson’s Correlation: To assess relationships between staffing levels, work schedules, overtime, and turnover with burnout, job satisfaction, and intention to leave.
2. Multiple Regression Analysis: To determine the predictive strength of the independent variables on burnout, job satisfaction, and intention to leave.
3. ANOVA and t-tests: To compare group differences (e.g., between professional roles or departments).
Ethical Considerations
Ethical approval for the study was obtained from the relevant Institutional Review Board (IRB). All participants were informed about the study’s purpose, ensured of their anonymity, and advised of their right to withdraw at any time without penalty. Data were stored securely and used solely for research purposes.
Limitations
The cross-sectional design limited the ability to establish causation. Selfreported data may have introduced response bias. However, anonymity and validated instruments were used to mitigate these concerns.
Results
Participants’ Characteristics
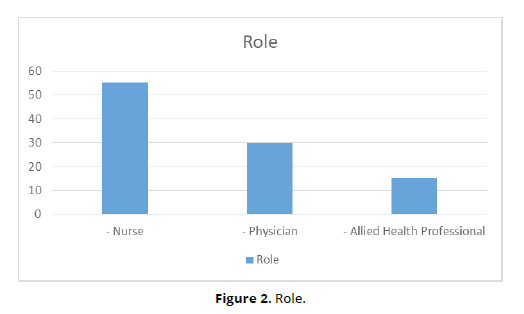
A total of 400 healthcare workers participated in the study. The demographic and professional characteristics of the participants are summarized in Table 1. Most participants were female (65%), nurses made up the majority (55%), and the mean years of experience were 8.2 years (SD = 4.5) (Table 1) (Figure 1-3).
| Characteristic | Frequency (n = 400) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 140 | 35 |
| Female | 260 | 65 |
| Role | ||
| Nurse | 220 | 55 |
| Physician | 120 | 30 |
| Allied Health Professional | 60 | 15 |
| Years of Experience | ||
| Less than 5 years | 120 | 30 |
| 5–10 years | 180 | 45 |
| More than 10 years | 100 | 25 |
Staffing Levels and Work Schedules
Staffing levels and work schedules were evaluated based on the number of patients per shift and hours worked per week. Table 2 demonstrates the distribution of these variables. Over 70% of participants reported handling more than five patients per shift, and 62% worked more than 40 hours per week (Table 2) (Figure 4, 5).
| Variable | Frequency (n = 400) | Percentage (%) |
|---|---|---|
| Patients per Shift | ||
| - 1–3 patients | 60 | 15 |
| - 4–5 patients | 60 | 15 |
| - More than 5 patients | 280 | 70 |
| Hours Worked per Week | ||
| - Less than 40 hours | 152 | 38 |
| - More than 40 hours | 248 | 62 |
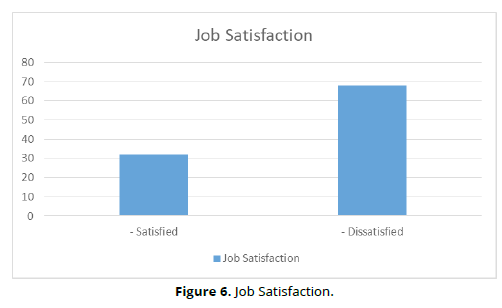
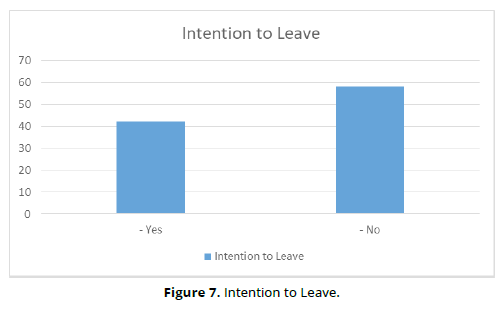
Burnout, Job Satisfaction, and Intention to Leave
The mean burnout score based on the Maslach Burnout Inventory (MBI) was 38.7 (SD = 9.3), indicating moderate levels of burnout. Job satisfaction scores were generally low, with 68% of participants reporting dissatisfaction.
Additionally, 42% of healthcare workers indicated a strong intention to leave their current position within the next year (Table 3) (Figure 6, 7).
| Outcome Measure | Mean (SD) or Frequency | Percentage (%) |
|---|---|---|
| Burnout (MBI Score) | 38.7 (SD = 9.3) | - |
| - Satisfied | 128 | 32 |
| - Dissatisfied | 272 | 68 |
| Intention to Leave | ||
| - Yes | 168 | 42 |
| - No | 232 | 58 |
Relationships Among Variables
Pearson’s correlation analysis revealed significant positive correlations between staffing levels (patients per shift) and burnout scores (r = 0.45, p < 0.01). Similarly, long work hours and required overtime were significantly associated with higher burnout (r = 0.39, p < 0.01) and lower job satisfaction (r = -0.42, p < 0.01). Table 4 summarizes the regression analysis results, highlighting the predictive effects of staffing levels, work schedules, and required overtime on burnout, job satisfaction, and intention to leave (Table 4).
Predictor Variable |
Burnout (β) | Job Satisfaction (β) | Intention to Leave (β) |
|---|---|---|---|
| Staffing Levels (Patients) | 0.45** | -0.35** | 0.32** |
| Work Hours (per Week) | 0.39** | -0.42** | 0.28** |
| Required Overtime | 0.41** | -0.33** | 0.31** |
The study found that higher patient loads, longer work hours, and required overtime significantly contributed to burnout among healthcare workers. These factors also decreased job satisfaction and increased the intention to leave their roles. Addressing these staffing and scheduling issues may help mitigate the negative outcomes for healthcare workers in acute care settings.
Discussion
This study investigated the impact of staffing levels, work schedules, and required overtime on burnout, job satisfaction, and intention to leave among healthcare workers in acute care hospitals. Our findings align with and extend prior research, highlighting critical challenges in hospital work environments and their implications for workforce well-being.
Burnout and Staffing Levels
Burnout levels were significantly correlated with higher patient loads and long work hours. This aligns with Shin et al. (2018), who found that insufficient among nurses, ultimately affecting the quality of care. Similarly, Bae (2021) reported that higher nurse-patient ratios are strongly associated with adverse nurse outcomes, including burnout.
The high patient-to-staff ratio observed in this study (70% of participants managing more than five patients per shift) underscores the urgent need to reassess staffing policies. Ensuring adequate staffing has been shown to reduce hospital-acquired conditions (Shin, Park, & Bae, 2019), which can indirectly mitigate burnout by improving job conditions and reducing workload.
Work Hours, Overtime, and Job Satisfaction
Our results indicate that extended work hours and required overtime are negatively associated with job satisfaction. This corroborates findings by Bae and Fabry (2014), who identified long shifts and mandatory overtime as predictors of lower job satisfaction and higher turnover intentions. Similarly, Gehri et al. (2023) found that irregular work schedules and extended hours in psychiatric hospitals significantly contribute to emotional exhaustion and intention to leave.
Healthcare workers in our study reported dissatisfaction at a rate of 68%, which is concerning given the relationship between job dissatisfaction and turnover. According to O’Brien-Pallas et al. (2010), turnover disrupts team dynamics, increases recruitment costs, and negatively impacts patient outcomes. Addressing scheduling issues, such as reducing overtime and providing more predictable work hours, could improve satisfaction and reduce attrition rates.
Intention to Leave and Turnover
Nearly half of the participants in this study (42%) expressed an intention to leave their current position, consistent with trends reported in Bae’s (2022) systematic review. High turnover intentions are often a response to chronic workplace stressors, including understaffing and extended hours. This finding is supported by Park et al. (2012), who developed a turnover intention model highlighting the mediating role of job dissatisfaction and burnout.
The economic and noneconomic costs of turnover, as detailed by Bae (2022), emphasize the need for proactive interventions. Strategies such as flexible scheduling, workload redistribution, and career development programs could mitigate turnover intentions and retain experienced staff.
Broader Implications and the Quality Framework
Donabedian’s (1980) framework of structure, process, and outcomes provides a useful lens for interpreting these findings. Structural deficiencies, such as insufficient staffing and poor schedule management, negatively influence care processes and outcomes for both patients and staff. Improving structural elements of the healthcare system, including staffing policies and scheduling practices, is essential to fostering a sustainable and satisfied workforce.
Strengths and Limitations
This study contributes to the growing body of evidence on healthcare workforce challenges by using a robust sample size and validated instruments. However, it is important to acknowledge the cross-sectional design, which precludes causal inferences. Additionally, self-reported data may be subject to bias, although the use of validated tools such as the Maslach Burnout Inventory and Copenhagen Psychosocial Questionnaire enhances the reliability of findings.
Future Directions
Future research should explore longitudinal designs to better understand the causal pathways linking staffing and scheduling practices to nurse outcomes. Investigating interventions, such as the implementation of flexible work hours and support programs, may provide actionable insights for healthcare administrators.
Conclusion
In conclusion, our study highlights the detrimental effects of inadequate staffing, extended work hours, and required overtime on healthcare workers’ burnout, job satisfaction, and turnover intentions. These findings underscore the need for systemic reforms in acute care hospitals to create supportive and sustainable work environments. By addressing these critical issues, healthcare institutions can enhance workforce well-being and improve the quality of care delivered to patients.
References
Brook J, Aitken L, Webb R, MacLaren J, Salmon D. Characteristics of Successful Interventions to Reduce Turnover and Increase Retention of Early Career Nurses: A Systematic Review. Int J Nurs Stud (2019) 91:47–59. 10.1016/j.ijnurstu.2018.11.003
World Health Organization. State of the World’s Nursing (2020). Available from: https://www.who.int/publications/i/item/9789240003279 (Accessed April 17, 2024).
International Council of Nurses. ICN Policy Brief-The Global Nursing Shortage and Nurse Retention (2021). Available from: https://www.icn.ch/sites/default/files/inline-files/ICN%20Policy%20Brief_Nurse%20Shortage%20and%20Retention.pdf (Accessed April 17, 2024).
Buchan JC, Howard SF. The Global Nursing Workforce and the COVID-19 Pandemic- A Report Commissioned by the International Centre on Nurse Migration (2022). Available from: https://www.icn.ch/sites/default/files/2023-04/Sustain%20and%20Retain%20in%202022%20and%20Beyond-%20The%20global%20nursing%20workforce%20and%20the%20COVID-19%20pandemic.pdf (Accessed April 17, 2024).
Nelson-Brantley HV, Park SH, Bergquist-Beringer S. Characteristics of the Nursing Practice Environment Associated With Lower Unit-Level RN Turnover. J Nurs Adm (2018) 48:31–7. 10.1097/NNA.0000000000000567
Kerzman H, Van Dijk D, Siman-Tov M, Friedman S, Goldberg S. Professional Characteristics and Work Attitudes of Hospital Nurses Who Leave Compared With Those Who Stay. J Nurs Manag (2020) 28:1364–71. 10.1111/jonm.13090
Organization for Economic Co-operation and Development. Healthcare Resources: Nurses (2021). Available from: https://stats.oecd.org/ (Accessed April 17, 2024).
Korea Hospital Nurses Association. A Survey on the Status of Hospital Nursing Personnel Assignment 2020 (2020).
Bae SH, Kelly M, Brewer CS, Spencer A. Analysis of Nurse Staffing and Patient Outcomes Using Comprehensive Nurse Staffing Characteristics in Acute Care Nursing Units. J Nurs Care Qual (2014) 29:318–26. 10.1097/NCQ.0000000000000057
Bourgon Labelle J, Audet LA, Farand P, Rochefort CM. Are Hospital Nurse Staffing Practices Associated With Postoperative Cardiac Events and Death? A Systematic Review. PLOS ONE (2019) 14:e0223979. 10.1371/journal.pone.0223979
Shin S, Park JH, Bae SH. Nurse Staffing and Hospital-Acquired Conditions: A Systematic Review. J Clin Nurs (2019) 28:4264–75. 10.1111/jocn.15046
Bae SH. Relationships Between Comprehensive Characteristics of Nurse Work Schedules and Adverse Patient Outcomes: A Systematic Literature Review. J Clin Nurs (2021) 30:2202–21. 10.1111/jocn.15728
Bae SH. Noneconomic and Economic Impacts of Nurse Turnover in Hospitals: A Systematic Review. Int Nurs Rev (2022) 69:392–404. 10.1111/inr.12769
Shin S, Park JH, Bae SH. Nurse Staffing and Nurse Outcomes: A Systematic Review and Meta-Analysis. Nurs Outlook (2018) 66:273–82. 10.1016/j.outlook.2017.12.002
Bae SH. Intensive Care Nurse Staffing and Nurse Outcomes: A Systematic Review. Nurs Crit Care (2021) 26:457–66. 10.1111/nicc.12588
Bae SH, Fabry D. Assessing the Relationships Between Nurse Work Hours/Overtime and Nurse and Patient Outcomes: Systematic Literature Review. Nurs Outlook (2014) 62:138–56. 10.1016/j.outlook.2013.10.009
O’Brien-Pallas L, Murphy GT, Shamian J, Li X, Hayes LJ. Impact and Determinants of Nurse Turnover: A Pan-Canadian Study. J Nurs Manag (2010) 18:1073–86. 10.1111/j.1365-2834.2010.01167.x
Gehri B, Bachnick S, Schwendimann R, Simon M. Work-Schedule Management in Psychiatric Hospitals and Its Associations With Nurses' Emotional Exhaustion and Intention to Leave: A Cross-Sectional Multicenter Study. Int J Nurs Stud (2023) 146:104583. 10.1016/j.ijnurstu.2023.104583
Donabedian A. The Definition of Quality and Approaches to Its Assessment. Ann Arbor, MI: Health Administration Press; (1980).
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav Res Methods (2007) 39:175–91. 10.3758/bf03193146
June KJ, Choi ES. Reliability and Validity of the Korean Version of the Copenhagen Psyco-Social Questionnaire Scale. Korean J Occup Health Nurs (2013) 22:1–12. 10.5807/kjohn.2013.22.1.1
Pejtersen JH, Kristensen TS, Borg V, Bjorner JB. The Second Version of the Copenhagen Psychosocial Questionnaire. Scand J Public Health (2010) 38:8–24. 10.1177/1403494809349858
Lawler EE. Satisfaction and Behavior. 2nd ed. McGraw-Hill; (1983).
Park KO, Kim JK, Kim SY, Chang S. A Model on Turnover Intention of Chief Nurse Officers. J Korean Acad Nurs (2012) 42:9–18. 10.4040/jkan.2012.42.1.9
Kim SH, Lee TW. Study of the Relationship Between Compassion Fatigue, Somatization and Silencing Response Among Hospital Nurses: Focusing on the Mediating Effects of Silencing Response. Korean J Adult Nurs (2014) 26:362. 10.7475/kjan.2014.26.3.362