Research Article - (2024) Volume 19, Issue 3
*Correspondence: Dr. Ishraq Yousef Abdul Kareem Al-Tarawneh, Counseling Psychology Ishraqat Center for Scientific Consulting, Jordan, Email:
Abstract
Menstrual disorders, hormonal imbalances, and mood disturbances are interconnected aspects of women's health that can significantly impact daily life and well-being. Menstrual disorders encompass a range of irregularities in the menstrual cycle, such as irregular periods, heavy bleeding (menorrhagia), painful periods (dysmenorrhea), and absence of menstruation (amenorrhea). These disorders can stem from various factors, including hormonal imbalances, stress, lifestyle factors, and underlying medical conditions. This study investigates the predictive ability of menstrual disorders and hormonal imbalances in the development of mood disorders in females. To achieve the study objectives, a questionnaire was developed using Google Forms and distributed via social media to a random sample of 500 female students at the University of Jordan. Using statistical analysis software (SPSS), the study concluded that the majority of student's experience moderate to severe symptoms of menstrual disorders, with the most common and severe symptoms being abdominal pain. In addition, across various domains such as menstrual disorders, changes in weight, skin changes, fatigue, mood changes, sleep problems, and digestive issues, a significant proportion of student's report experiencing moderate to severe symptoms. The results showed that also significant proportions of students experiencing various symptoms indicative of mood disorders. besides, the study revealed a correlation between menstrual disorders and hormonal imbalance with mood disturbances among females. The study recommended the development of education and awareness programs aimed at addressing menstrual disorders and hormonal imbalances among females. Additionally, it suggested the provision of specialized healthcare services to better manage and treat these conditions
Keywords
menstrual disorders, hormonal imbalances, mood disorders.
Introduction
Mood disorders, encompassing a range of affective conditions such as depression, anxiety, and bipolar disorder, represent a significant public health concern due to their prevalence and impact on the quality of life. Understanding the multifaceted etiology of mood disorders is crucial for effective prevention and treatment. Among the various biological, psychological, and social factors implicated in mood disorders, menstrual disorders and hormonal imbalances in females have garnered increasing attention (Özge et.al,2023).
Menstrual disorders, including dysmenorrhea (painful menstruation), premenstrual syndrome (PMS), and premenstrual dysphoric disorder (PMDD), are prevalent among women of reproductive age. Dysmenorrhea affects a significant portion of women, often leading to absenteeism and reduced quality of life. PMS, characterized by a variety of physical and emotional symptoms occurring in the luteal phase of the menstrual cycle, affects up to 75% of menstruating women to varying degrees. PMDD, a severe form of PMS, is marked by debilitating mood disturbances such as severe irritability, depression, and anxiety (Chekol, A. T., Reta, Y., Ayinewa, F., Hailu, L., Tesema, M., & Wale, M. A. 2024).
The cyclical nature of these menstrual disorders suggests a potential link between the menstrual cycle and mood fluctuations. Research indicates that hormonal changes during the menstrual cycle, particularly fluctuations in estrogen and progesterone, can significantly impact neurotransmitter systems associated with mood regulation, including serotonin and gamma-aminobutyric acid (GABA). Consequently, menstrual disorders characterized by hormonal dysregulation may serve as important predictors of mood disorders(Rugvedh, P., Gundreddy, P., & Wandile, B. 2023).
Hormonal imbalances extend beyond the menstrual cycle and include conditions such as polycystic ovary syndrome (PCOS), thyroid dysfunction, and menopause. PCOS, affecting approximately 10% of women of reproductive age, is characterized by hyper and organism, ovulatory dysfunction, and polycystic ovaries. Women with PCOS are at an increased risk of developing mood disorders, including depression and anxiety. Thyroid dysfunction, encompassing both hyperthyroidism and hypothyroidism, is also closely linked to mood disturbances. Hypothyroidism, in particular, is associated with depressive symptoms, while hyperthyroidism is often linked to anxiety and agitation(.Witchel, S. F., Oberfield, S. E., & Peña, A. S. 2019).
Menopause, marking the end of reproductive life, brings significant hormonal changes, particularly a decline in estrogen levels. This transition is associated with an increased risk of developing mood disorders, including major depressive disorder and anxiety. The hormonal changes during menopause can affect the hypothalamic-pituitary-adrenal (HPA) axis, further contributing to mood instability (Alblooshi, S., Taylor, M., & Gill, N. 2023).
Hormones play a critical role in regulating mood by influencing neurotransmitter systems. Estrogen, for example, modulates the serotonergic system, enhancing serotonin synthesis and receptor sensitivity. Progesterone and its metabolites, on the other hand, interact with the GABAergic system, producing calming effects. Imbalances in these hormones can disrupt these neurotransmitter systems, leading to mood disturbances(Hwang, W. J., Lee, T. Y., Kim, N. S., & Kwon, J. S. 2020).
The HPA axis, a central stress response system, is also influenced by hormonal changes. Chronic stress and dysregulation of the HPA axis can lead to alterations in cortisol levels, which are linked to both menstrual disorders and mood disorders. Elevated cortisol levels, commonly seen in chronic stress, can contribute to the development of mood disorders by affecting neurotransmitter systems and neuroplasticity(Stephens, M. A., & Wand, G. 2012).
Research Significance
Understanding the predictive ability of menstrual disorders and hormonal imbalances in mood disorders is crucial for developing targeted interventions. This research holds several significant Implications for both clinical practice and public health:
Personalized Treatment Strategies: Early identification of women at risk for mood disorders based on their menstrual and hormonal profiles could lead to more personalized and effective treatment strategies. By recognizing specific hormonal patterns and menstrual irregularities associated with mood disturbances, healthcare providers can tailor interventions that address these underlying biological factors. This personalized approach may improve treatment outcomes and reduce the trial-and-error process often associated with managing mood disorders.
Preventive Measures: Identifying predictive markers in menstrual and hormonal profiles allows for the implementation of preventive measures. Women who exhibit signs of hormonal imbalances or menstrual disorders can be monitored more closely for the development of mood disorders. Preventive strategies, such as lifestyle modifications, stress management techniques, and hormonal therapies, can be introduced earlier, potentially mitigating the severity or even preventing the onset of mood disorders.
Improved Diagnostic Accuracy: Understanding the link between menstrual disorders, hormonal imbalances, and mood disorders can enhance diagnostic accuracy. Clinicians can consider menstrual and hormonal factors when assessing women presenting with mood symptoms, leading to a more comprehensive evaluation. This holistic approach ensures that all relevant factors are taken into account, reducing the likelihood of misdiagnosis and enabling more accurate and timely treatment.
Destigmatization and Awareness: This research could contribute to the destigmatization of mood disorders in women by highlighting the biological underpinnings of these conditions. By emphasizing that mood disorders can be influenced by hormonal and menstrual factors, it challenges the notion that these conditions are solely psychological or a result of personal weakness. Increased awareness and understanding can foster a more supportive environment for women to seek help without fear of judgment.
Educational and Public Health Initiatives: The findings from this research can inform educational programs and public health initiatives aimed at promoting women's mental health. Awareness campaigns can educate women about the potential impact of menstrual and hormonal health on mood, encouraging them to seek medical advice for menstrual irregularities or mood symptoms. Public health policies can be developed to ensure that hormonal and menstrual health is integrated into routine health screenings and mental health assessments.
Research and Clinical Advancements: This research lays the groundwork for future studies exploring the complex interactions between hormones, menstrual health, and mood. It can lead to the development of new diagnostic tools and treatment modalities that specifically address the hormonal and menstrual dimensions of mood disorders. Such advancements can significantly improve the standard of care for women affected by these conditions.
Objectives of the Study
This research aims to:
Investigate the prevalence and severity of mood disorders in women with menstrual disorders and hormonal imbalances.
Examine the specific hormonal changes associated with mood disturbances.
Explore the interplay between hormonal fluctuations and neurotransmitter systems in mood regulation.
Develop predictive models for mood disorders based on menstrual and hormonal profiles.
Study Problem
The problem addressed by this study is the high prevalence of mood disorders among females and the potential under-recognition of menstrual disorders and hormonal imbalances as significant contributing factors. Mood disorders, such as depression and anxiety, significantly impact the quality of life, productivity, and overall well-being of women. However, the link between menstrual health, hormonal fluctuations, and mood disturbances is often over looked in both clinical practice and research. This gap in understanding hinders the development of effective, targeted interventions that could alleviate mood disorders and improve mental health outcomes for women.
To address this problem, the study aims to explore the predictive ability of menstrual disorders and hormonal imbalances in the development and severity of mood disorders in females. The specific research questions guiding this study are:
Prevalence and Severity
What is the prevalence of mood disorders among women with menstrual disorders such as dysmenorrhea, premenstrual syndrome (PMS), and premenstrual dysphoric disorder (PMDD)?
How severe are the mood disorders experienced by women with these menstrual disorders compared to those without?
Hormonal Changes and Mood Disturbances
What specific hormonal changes are associated with mood disturbances in women with menstrual disorders and hormonal imbalances?
How do fluctuations in estrogen, progesterone, and other relevant hormones correlate with the onset and severity of mood disorders?
Interplay Between Hormones and Neuro transmitters
How do hormonal fluctuations influence neurotransmitter systems involved in mood regulation, such as serotonin and gamma-aminobutyric acid (GABA)?
What role does the hypothalamic-pituitary-adrenal (HPA) axis play in mediating the relationship between hormonal changes and mood disorders?
Predictive Models
Can specific menstrual and hormonal profiles be identified that predict the likelihood of developing mood disorders?
How accurate are these predictive models in forecasting mood disorders in women with varying menstrual and hormonal conditions?
Impact of Interventions
What interventions can effectively address menstrual and hormonal factors to prevent or reduce mood disorders in women?
How do personalized treatment strategies based on menstrual and hormonal profiles compare to standard treatments in terms of efficacy?
Literature Review
Mood disorders, including depression, anxiety, and bipolar disorder, are prevalent and debilitating conditions that significantly impact women's mental health and quality of life. An increasing body of evidence suggests a strong link between mood disorders and biological factors unique to women, such as menstrual disorders and hormonal imbalances.
Menstrual Disorders and Mood Disorders.
Dysmenorrhea
Dysmenorrhea, commonly known as painful menstruation, is one of the most prevalent menstrual disorders affecting women of reproductive age. It is classified into two types: primary dysmenorrhea, which occurs in the absence of any pelvic pathology, and secondary dysmenorrhea, which is associated with underlying conditions such as endometriosis or fibroids. Dysmenorrhea is characterized by cramping pain in the lower abdomen, which can be severe and debilitating, often accompanied by symptoms such as nausea, vomiting, fatigue, and headaches (Itani, R., Soubra, L., Karout, S., Rahme, D., Karout, L., & Khojah, H. M. J. 2022).
Prevalence and Impact
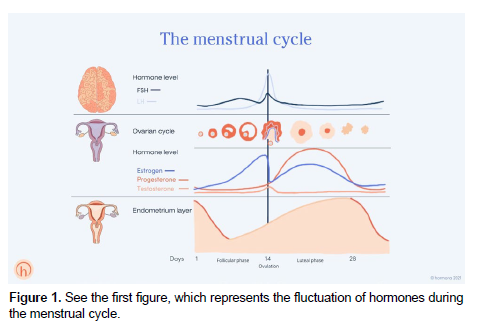
Dysmenorrhea affects a significant portion of the female population, with estimates suggesting that up to 90% of adolescent girls and women experience some degree of menstrual pain. Among these, approximately 10-20% report severe symptoms that interfere with daily activities and quality of life. The high prevalence of dysmenorrhea highlights its importance as a public health issue and underscores the need for effective management strategies (Deborah, et. al, 2024) (Figure 1).
Figure 1 represents many aspects, but the first aspect indicates that hormonal disorders are directly affected by the nervous center in the brain, which is primarily responsible for mood swings in females during the menstrual cycle. It is also noted that hormones are stable in females until the time of the menstrual cycle, and these hormones become at their highest level during The first days of the menstrual cycle, which is shown in the stages of hormones in the previous figure.
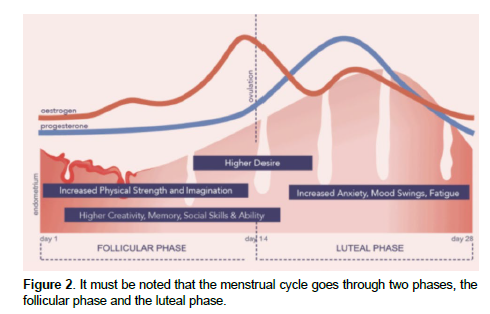
It must be noted that the menstrual cycle goes through two phases, the follicular phase and the luteal phase (Figure 2).
The second figure is closely related to the first figure, and it shows the two basic phases of the menstrual cycle. The follicular phase begins on the first day of menstruation and ends with ovulation. It typically lasts about 14 days but can vary among individuals.
Hormonal Changes
Estrogen: During the follicular phase, estrogen levels gradually rise as the follicles in the ovaries develop. The increase in estrogen stimulates the growth of the endometrial lining of the uterus, preparing it for potential implantation of a fertilized egg.
Follicle-Stimulating Hormone (FSH): FSH is secreted by the pituitary gland and promotes the growth of ovarian follicles. Several follicles begin to mature, but usually only one becomes the dominant follicle that will be released during ovulation.
Mood and Psychological Effects
The rising estrogen levels during the follicular phase have been associated with positive effects on mood and cognitive function. Estrogen enhances the production and activity of neurotransmitters such as serotonin and dopamine, which are crucial for mood regulation and overall mental well-being. Women often report feeling more energetic, positive, and focused during this phase of the menstrual cycle.
The luteal phase begins after ovulation and lasts until the onset of menstruation, typically around 14 days.
Hormonal Changes
Progesterone: Following ovulation, the corpus luteum (the remnant of the dominant follicle) secretes progesterone, which works to maintain the endometrial lining. Progesterone levels peak in the middle of the luteal phase and then decline if pregnancy does not occur.
Estrogen: While progesterone is the dominant hormone in the luteal phase, estrogen levels also remain elevated initially and then gradually decrease towards the end of the cycle.
Mood and Psychological Effects
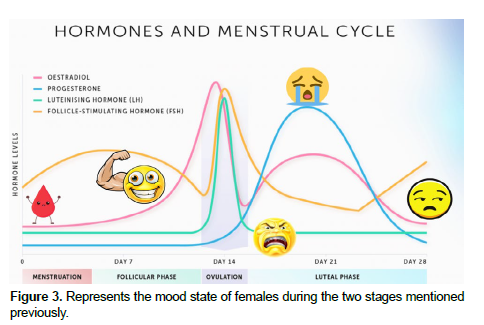
The luteal phase is often associated with mood fluctuations and emotional disturbances, particularly in women who experience premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD). The decline in estrogen and the rise and subsequent fall of progesterone can lead to symptoms such as irritability, depression, anxiety, and mood swings (Figure 3).
The previous figure Highlights the two phases of the menstrual cycle. It is clear from the above that the female in the first period of the menstrual cycle is in ideal health, but hormones begin to affect the mood starting from the luteal phase, and thus the condition changes radically from happiness to a fluctuating mood until the end of the menstrual cycle.
The brain and hormones during the menstrual cycle.
The menstrual cycle involves complex interactions between the brain and the endocrine system, leading to significant hormonal fluctuations that can affect both physical and mental health. Understanding how the brain and hormones interact during the menstrual cycle can provide insights into the mechanisms underlying mood changes and other psychological symptoms that many women experience.
The Hypothalamic-Pituitary-Ovarian (HPO) Axis
The regulation of the menstrual cycle is primarily controlled by the hypothalamic-pituitary-ovarian (HPO) axis, which involves a coordinated series of hormonal signals between the hypothalamus, the pituitary gland, and the ovaries )Zhao, J., Pan, H., Liu, Y., He, Y., Shi, H., & Ge, C. 2023 (Figure 4).
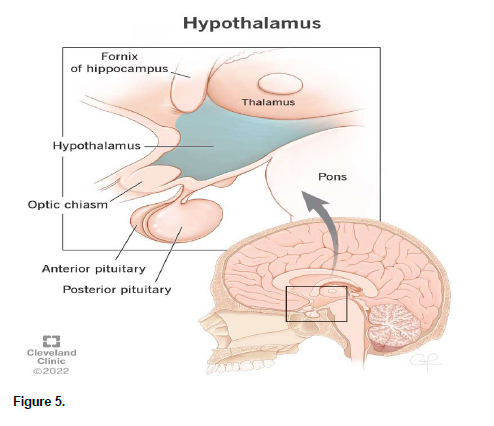
Hypothalamus
The hypothalamus is a small region at the base of the brain that plays a crucial role in hormone regulation. It releases gonadotropin-releasing hormone (GnRH) in a pulsatile manner, which is essential for the stimulation of the pituitary gland (Cleveland Clinic). (Figure 5).
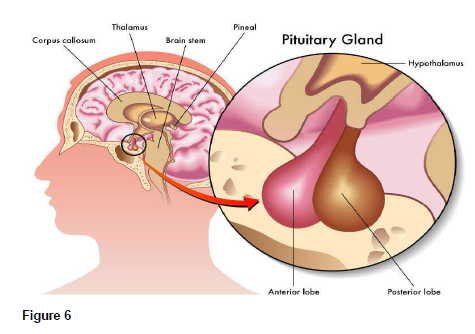
Pituitary Gland
The anterior pituitary gland responds to GnRH by secreting two key hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH promotes the growth and maturation of ovarian follicles, while LH triggers ovulation and the formation of the corpus luteum (healthdirect) (Figure 6).
Ovaries
The ovaries produce estrogen and progesterone in response to FSH and LH. These hormones not only regulate the menstrual cycle but also have widespread effects on the brain and behavior (britannica) (Figure 7).
Hormonal fluctuations and brain function
As we mentioned previously, the menstrual cycle is divided into two main phases: the follicular phase and the luteal phase, each of which is characterized by distinct hormonal characteristics that affect brain functions.
Follicular phase
During the follicular phase, estrogen levels gradually rise as ovarian follicles develop. Estrogen has several effects on the brain:
Modulating neurotransmitters: Estrogen enhances the activity of neurotransmitters such as serotonin, dopamine, and norepinephrine, which are essential for regulating mood. It increases serotonin synthesis and receptor sensitivity, which contributes to improved mood and cognitive function.
Neuroprotection: Estrogen has neuroprotective properties, promoting nerve cell growth and survival. It also enhances synaptic plasticity, which is important for learning and memory.
Cognitive function: High estrogen levels during the follicular phase are associated with enhanced cognitive performance, including improved verbal and executive memory.
Luteal Phase
The luteal phase is characterized by the rise in progesterone levels following ovulation. Progesterone, along with continuing but fluctuating levels of estrogen, plays a significant role in preparing the body for potential pregnancy and also affects brain function and mood.
Neurotransmitter Modulation: Progesterone and its metabolite, allopregnanolone, have a calming effect on the brain by enhancing the activity of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter. This can lead to feelings of relaxation and reduced anxiety. However, in some women, these changes can also contribute to mood swings, irritability, and depression, particularly as progesterone levels drop towards the end of the luteal phase.
Stress Response: Progesterone can influence the hypothalamic-pituitary-adrenal (HPA) axis, which is involved in the body's stress response. Fluctuations in progesterone levels may affect cortisol production and stress reactivity, potentially exacerbating symptoms of anxiety and depression.
Mood Changes: The combination of declining estrogen and fluctuating progesterone levels during the luteal phase is often associated with premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD). Symptoms can include irritability, mood swings, depression, anxiety, and physical symptoms such as bloating and fatigue.
Hormonal Influence on Brain Regions
Hormones such as estrogen and progesterone influence several brain regions involved in emotion regulation, cognitive function, and stress response.
Amygdala: The amygdala is involved in emotional processing and stress responses. Estrogen and progesterone can modulate the activity of the amygdala, influencing emotional reactivity and mood. During the luteal phase, changes in these hormones can lead to heightened emotional responses and mood swings.
Prefrontal Cortex: The prefrontal cortex is critical for executive functions, decision-making, and impulse control. Estrogen enhances prefrontal cortex function, which can improve cognitive abilities and mood stability during the follicular phase.
Hippocampus: The hippocampus is essential for memory formation and regulation of the stress response. Estrogen promotes neurogenesis and synaptic plasticity in the hippocampus, supporting cognitive function and resilience to stress.
Neurobiological Mechanisms
The interaction between hormones and neurotransmitter systems underpins the neurobiological mechanisms linking the menstrual cycle to mood and cognitive changes.
Serotonin System: Estrogen increases the synthesis of serotonin, enhances the sensitivity of serotonin receptors, and inhibits serotonin reuptake. This leads to higher levels of serotonin in the brain, which is associated with improved mood and reduced anxiety.
GABAergic System: Progesterone and its metabolite allopregnanolone enhance GABAergic activity, producing anxiolytic and sedative effects. However, abrupt changes in progesterone levels can lead to mood disturbances in susceptible individuals.
HPA Axis: Hormonal fluctuations during the menstrual cycle can affect the HPA axis, influencing cortisol production and stress reactivity. Dysregulation of the HPA axis is linked to mood disorders such as depression and anxiety.
Clinical Implications
Understanding the interplay between the brain and hormones during the menstrual cycle has important clinical implications for the management of mood disorders in women.
Personalized Treatment: Recognizing the role of hormonal fluctuations in mood disorders can lead to more personalized treatment approaches. Hormone therapy, lifestyle modifications, and targeted pharmacological interventions can be tailored to address specific hormonal imbalances and their impact on mood.
Early Intervention: Identifying women at risk for severe mood disturbances related to the menstrual cycle can facilitate early intervention and preventive measures, potentially reducing the severity and duration of mood disorders.
Holistic Approach: A comprehensive approach that considers both biological and psychosocial factors is essential for effectively managing mood disorders in women. Integrating hormonal, psychological, and behavioral therapies can improve overall treatment outcomes.
Previous studies.
There are many previous studies that addressed the subject of the study:
Study of Balsom, A. A., & Gordon, J. L. (2021).
Objectives: Infertility is disproportionately associated with distress in women yet there has been limited research focusing on the relationship between coping strategies and fertility-monitoring techniques on distress in women struggling to conceive naturally.
Methods: Fifty-eight distressed women with infertility were recruited via social media. Every second day women's depressive and anxious mood was assessed in the morning and again in the evening along with their psychological coping strategies, the use of fertility monitoring techniques, and Fertility Quality of Life emotion subscale, over the course of one full menstrual cycle.
Results: During menstruation and statistically adjusting for morning depressive mood, active coping (β(SE) = -1.35 (0.36), p < .001) and behavioural engagement (β(SE) = -0.98 (0.35), p =.006) were associated with less depressive mood in the evening. Across all phases, social support seeking was associated with greater anxiety (β(SE) = 0.50 (0.20), p = .013) and lower emotional quality of life (β(SE) = -0.82 (0.32), p = .011). Use of fertility monitoring techniques was associated with heightened anxiety (M(SE) = 6.7 (0.2) vs. 5.9 (0.2), p < .001). The use of avoidance strategies (β(SE) = 3.22 (1.29), p = .016), endorsement of optimism (β(SE) = -4.72 (1.78), p = .011) and social support seeking (β(SE) = 3.09 (1.18), p = .012) throughout the cycle were significantly predictive of depression ratings following a negative pregnancy test, despite statistically adjusting for mean depression ratings throughout the menstrual cycle.
Conclusion: These findings highlight a number of cognitive and behavioural strategies that could be manipulated via psychological interventions to improve distress among women struggling to conceive.
Study of Alateeq, D., Binsuwaidan, L., Alazwari, L., Algarni, M., Al Hussain, M., Alzahrani, R., & Aljohani, R. (2022).
This study aims to explore the prevalence of dysmenorrhea and investigate its correlation with depressive symptoms among Princess Nourah bint Abdulrahman University (PNU) students. All participants (N = 487) in this cross-sectional study provided sociodemographic data, menstrual and medical history, and completed the Patient Health Questionnaire (PHQ-9) scale and (working ability, location, intensity, days of pain, dysmenorrhea [WaLIDD]) scale on a self-administered online questionnaire.
Results: The mean age of the females was 20.64 ± 2.38 years, and 40.7% were from health colleges. Severe dysmenorrhea requiring medical attention and pain killers or herbs was reported by 30.8% of the students. Significant predictors of severe dysmenorrhea were: younger age, earlier menarche, pain killers and herbs used for menstrual pain, a doctor visit for menstrual pain, and depression. In addition, significant protective factors of depression were: later menarche age, having a regular menstrual cycle, and longer duration.
Conclusions: Students with severe dysmenorrhea have a higher risk of depression than other students. The findings stress the importance of awareness, education, a multidisciplinary approach to women's health, and early detection to prevent future complications.
Study of Handy, A. B., Greenfield, S. F., Yonkers, K. A., & Payne, L. A. (2022).
The researchers in this study synthesized the literature examining the worsening of a variety of psychological symptoms across the menstrual cycle in adult women. Results showed that the premenstrual and menstrual phases were most consistently implicated in worsening symptoms across diagnosis. Specifically, strong evidence suggests an increase in the incidence of psychosis, mania, depression, suicide attempts, and alcohol abuse during these stages. Anxiety, stress, and binge eating appear to be generally high throughout the luteal phase. The subjective effects of smoking and cocaine use are reduced during the luteal phase, but less data are available for other substances. Less consistent patterns have been demonstrated for panic disorder, PTSD symptoms, and borderline personality disorder, and it is difficult to draw conclusions about symptoms of generalized anxiety disorder, social anxiety disorder, obsessive-compulsive disorder, and trichotillomania due to limited data. . Future research should focus on developing standardized methods for defining menstrual cycle phases and tailoring pharmacological and behavioral interventions to manage fluctuations in psychological symptoms across the menstrual cycle.
Study of Hromatko, I., & Mikac, U. (2023).
The aim of this prospective study was to compare both the positive and negative dimensions of mood across the menstrual cycle. A group of 60 healthy, normally cycling women assessed their mood throughout three phases of their menstrual cycles: the early follicular (low estradiol and progesterone), the late follicular (fertile phase; high estradiol, low progesterone) and the mid-luteal phase (high levels of both estradiol and progesterone). Repeated MANOVA evaluations showed a significant increase in positive (friendly, cheerful, focused, active) and a significant decrease in negative (anxious, depressed, fatigued, hostile) dimensions of mood mid-cycle, i.e., during the late follicular phase (η2 = 0.072−0.174, p < 0.05). Contrary to the widespread belief that negative moods are characteristic of the luteal phase (preceding the onset of the next cycle), the post hoc Bonferroni tests showed that none of the mood dimensions differed between the mid-luteal and early follicular phases of the cycle. The results held when controlling for relationship status and order of testing. This pattern of fluctuations is in accordance with the ovulatory-shift hypothesis, i.e., the notion that the emotions of attraction rise during a short window during which the conception is likely.
Methodology and Procedures
Study Approach
The current study employed a descriptive correlational approach to examine the predictive ability of menstrual disorders and hormonal imbalance on the level of mood disorders in females.
Population and Sample
The study population comprises female students at the University of Jordan during the academic year 2023-2024 (N= 30,442). Using random sampling method, a sample composed of 500 respondents was selected. the following table show the menstrual patterns of the respondents (Table 1).
| Freq. | Percentage% | ||
|---|---|---|---|
| Age of respondents | <20 | 153 | 30.6 |
| 20-24 | 286 | 57.2 | |
| ≥25 | 61 | 12.2 | |
| Age at menarche | <12 | 13 | 2.6 |
| 12-15 | 214 | 42.8 | |
| 16-18 | 254 | 50.8 | |
| >18 | 19 | 3.8 | |
| Duration of flow | <2 | 11 | 2.2 |
| 2-4 | 213 | 42.6 | |
| 5-7 | 256 | 51.2 | |
| >8 | 20 | 4 | |
| Amount of flow | Little | 168 | 33.6 |
| Moderate | 271 | 54.2 | |
| Heavy | 61 | 12.2 | |
| Cycle Length | ≤20 | 10 | 2 |
| 21-35 | 448 | 89.6 | |
| ≥36 | 42 | 8.4 | |
| Painful menstrual flow (dysmennorhea) | Yes | 201 | 40.2 |
| No | 299 | 59.8 |
Study Instrument
The researcher designed a questionnaire by Google forms and distributed it electronically using social media to reach the targeted sample. The instrument comprised four parts: the first part was dedicated to information regarding the menstrual cycle of the respondents, the second part included items related to menstrual disorders, the third part contained items about the symptoms of hormonal imbalance in females, and the fourth part included items related to mood disorders. To ensure the validity of the study instrument, it was reviewed by several specialists in the fields of psychology, medicine, and nursing from the faculty members of Jordanian universities. Based on the specialists' modifications. Regarding the reliability of the instrument, the Cronbach's alpha coefficient for the study domains was extracted, which amounted to (0.71, 0.84, 0.81, 0.77) respectively (Table 2).
| Symptoms | Does Not Occur | Mild | Moderate | Severe | Mean | STD | |
|---|---|---|---|---|---|---|---|
| Abdominal pain | Frq. | 12 | 4 | 254 | 230 | 3.40 | 0.63 |
| % | 2.4 | 0.8 | 50.8 | 46.0 | |||
| Back pain | Frq. | 0 | 12 | 199 | 289 | 3.55 | 0.54 |
| % | 0 | 2.4 | 39.8 | 57.8 | |||
| Headache | Frq. | 0 | 98 | 248 | 154 | 3.11 | 0.70 |
| % | 0 | 19.6 | 49.6 | 30.8 | |||
| Abdominal bloating | Frq. | 6 | 21 | 209 | 264 | 3.46 | 0.64 |
| % | 1.2 | 4.2 | 41.8 | 52.8 | |||
| Fatigue and tiredness | Frq. | 12 | 30 | 140 | 318 | 3.53 | 0.72 |
| % | 2.4 | 6.0 | 28.0 | 63.6 | |||
| Breast pain | Frq. | 17 | 90 | 216 | 177 | 3.11 | 0.81 |
| % | 3.4 | 18.0 | 43.2 | 35.4 | |||
| Breast swelling | Frq. | 184 | 102 | 74 | 140 | 2.34 | 1.23 |
| % | 36.8 | 20.4 | 14.8 | 28.0 | |||
| Dizziness or lightheadedness | Frq. | 330 | 95 | 21 | 54 | 1.60 | 0.99 |
| % | 66.0 | 19.0 | 4.2 | 10.8 | |||
| Constipation | Frq. | 182 | 47 | 98 | 173 | 2.52 | 1.29 |
| % | 36.4 | 9.4 | 19.6 | 34.6 | |||
| Diarrhea | Frq. | 122 | 63 | 191 | 124 | 2.63 | 1.10 |
| % | 24.4 | 12.6 | 38.2 | 24.8 | |||
| Nausea | Frq. | 229 | 80 | 116 | 75 | 2.07 | 1.13 |
| % | 45.8 | 16.0 | 23.2 | 15.0 | |||
| Vomiting | Frq. | 278 | 69 | 66 | 87 | 1.92 | 1.18 |
| % | 55.6 | 13.8 | 13.2 | 17.4 | |||
| Changes in appetite (increase or decrease) | Frq. | 140 | 23 | 157 | 180 | 2.75 | 1.21 |
| % | 28.0 | 4.6 | 31.4 | 36.0 | |||
| Pain during urination | Frq. | 141 | 45 | 128 | 186 | 2.72 | 1.23 |
| % | 28.2 | 9.0 | 25.6 | 37.2 | |||
| Difficulty in focusing | Frq. | 118 | 75 | 161 | 146 | 2.67 | 1.13 |
| % | 23.6 | 15.0 | 32.2 | 29.2 |
Menstrual Disorders
The frequencies, percentages, arithmetic mean, and standard deviation of the students' responses regarding the extent of their suffering from menstrual disorders were extracted.
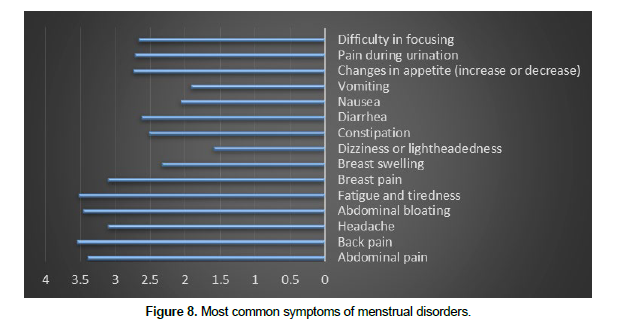
The data indicates that the majority of student's experience moderate to severe symptoms of menstrual disorders, with the most common and severe symptoms being abdominal pain (mean: 3.40, SD: 0.63), back pain (mean: 3.55, SD: 0.54), fatigue (mean: 3.53, SD: 0.72), and abdominal bloating (mean: 3.46, SD: 0.64). Symptoms like dizziness (mean: 1.60, SD: 0.99), nausea (mean: 2.07, SD: 1.13), and vomiting (mean: 1.92, SD: 1.18) are less commonly reported. The variations in mean scores and standard deviations highlight the different levels of impact these symptoms have on the students. These findings can be attributed to several factors. Physiological factors such as hormonal fluctuations and high prostaglandin levels can cause significant pain and discomfort. Lifestyle and health habits, including poor diet, lack of exercise, and high stress levels, can exacerbate these symptoms. Psychological factors like stress and emotional well-being also play a crucial role, as anxiety and depression can amplify the experience of menstrual discomfort. Additionally, underlying medical conditions such as endometriosis, polycystic ovary syndrome (PCOS), and uterine fibroids can lead to more severe symptoms. Environmental and social factors, such as limited access to healthcare and lack of education about menstrual health, further contribute to the severity of symptoms. Understanding these contributing factors is essential for developing effective strategies to manage and alleviate menstrual disorder symptoms among students. The following figure show most common symptoms of menstrual disorders (Figure 8).
Hormonal Imbalance
The frequencies, percentages, arithmetic mean, and standard deviation of the students' responses regarding the extent of symptoms of hormonal imbalance were extracted.
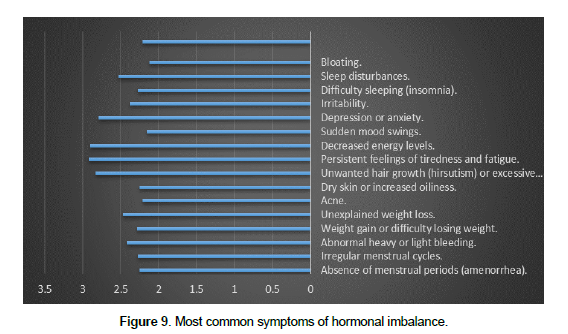
The data presented in Table (3) Highlights the substantial prevalence of symptoms related to hormonal imbalance among students. Across various domains such as menstrual disorders, changes in weight, skin changes, fatigue, mood changes, sleep problems, and digestive issues, a significant proportion of student's report experiencing moderate to severe symptoms. For instance, menstrual irregularities affect approximately 21.2% to 35.2% of students, while skin issues impact 36.8% to 75.0% at a moderate to severe level. These findings emphasize the pressing need for tailored interventions to address students' health concerns effectively. By recognizing the extent of these symptoms, educational institutions and healthcare providers can implement targeted strategies to alleviate the impact of hormonal imbalance, ultimately fostering a healthier and more supportive learning environment for students. The results are attributed to a multifactorial interaction related to female students, including hormonal changes, psychological and social pressures, lifestyle patterns, genetic factors, and university environment. These factors may interact with each other to determine the severity and prevalence of hormone-related symptoms among female students. The following figure show most common symptoms of hormonal imbalance (Figure 9).
| Symptoms | Does Not Occur | Mild | Moderate | Severe | Mean | STD | ||
|---|---|---|---|---|---|---|---|---|
| Menstrual Disorders: | Absence of menstrual periods (amenorrhea). | Frq. | 185 | 101 | 108 | 106 | 2.25 | 1.17 |
| % | 37.0 | 20.2 | 21.6 | 21.2 | ||||
| Irregular menstrual cycles. | Frq. | 151 | 176 | 60 | 113 | 2.27 | 1.12 | |
| % | 30.2 | 35.2 | 12.0 | 22.6 | ||||
| Abnormal heavy or light bleeding. | Frq. | 171 | 88 | 103 | 138 | 2.42 | 1.22 | |
| % | 34.2 | 17.6 | 20.6 | 27.6 | ||||
| Changes in Weight: | Weight gain or difficulty losing weight. | Frq. | 149 | 168 | 78 | 105 | 2.28 | 1.10 |
| % | 29.8 | 33.6 | 15.6 | 21.0 | ||||
| Unexplained weight loss. | Frq. | 114 | 130 | 163 | 93 | 2.47 | 1.04 | |
| % | 22.8 | 26.0 | 32.6 | 18.6 | ||||
| Skin Changes: | Acne. | Frq. | 201 | 93 | 105 | 101 | 2.21 | 1.17 |
| % | 40.2 | 18.6 | 21.0 | 20.2 | ||||
| Dry skin or increased oiliness. | Frq. | 167 | 149 | 74 | 110 | 2.25 | 1.14 | |
| % | 33.4 | 29.8 | 14.8 | 22.0 | ||||
| Unwanted hair growth (hirsutism) or excessive hair loss. | Frq. | 42 | 83 | 295 | 80 | 2.83 | 0.80 | |
| % | 8.4 | 16.6 | 59.0 | 16.0 | ||||
| Fatigue: | Persistent feelings of tiredness and fatigue. | Frq. | 97 | 48 | 151 | 204 | 2.92 | 1.13 |
| % | 19.4 | 9.6 | 30.2 | 40.8 | ||||
| Decreased energy levels. | Frq. | 94 | 46 | 176 | 184 | 2.90 | 1.10 | |
| % | 18.8 | 9.2 | 35.2 | 36.8 | ||||
| Mood Changes: | Sudden mood swings. | Frq. | 166 | 173 | 80 | 81 | 2.15 | 1.06 |
| % | 33.2 | 34.6 | 16.0 | 16.2 | ||||
| Depression or anxiety. | Frq. | 94 | 110 | 101 | 195 | 2.79 | 1.15 | |
| % | 18.8 | 22.0 | 20.2 | 39.0 | ||||
| Irritability. | Frq. | 168 | 99 | 108 | 125 | 2.38 | 1.19 | |
| % | 33.6 | 19.8 | 21.6 | 25.0 | ||||
| Sleep Problems: | Difficulty sleeping (insomnia). | Frq. | 186 | 108 | 89 | 117 | 2.27 | 1.19 |
| % | 37.2 | 21.6 | 17.8 | 23.4 | ||||
| Sleep disturbances. | Frq. | 138 | 104 | 114 | 144 | 2.53 | 1.17 | |
| % | 27.6 | 20.8 | 22.8 | 28.8 | ||||
| Digestive Issues: | Bloating. | Frq. | 189 | 142 | 89 | 80 | 2.12 | 1.09 |
| % | 37.8 | 28.4 | 17.8 | 16.0 | ||||
| Constipation or diarrhea. | Frq. | 230 | 50 | 103 | 117 | 2.21 | 1.25 | |
| % | 46 | 10 | 20.6 | 23.4 | ||||
Mood Disorders
The frequencies, percentages, arithmetic mean, and standard deviation of the students' responses regarding the extent of their suffering from mood disorders were extracted.
The data in Table (4) offers a comprehensive insight into the prevalence and severity of mood disorders among the surveyed students. It reveals significant proportions of students experiencing various symptoms indicative of mood disorders, with notable percentages reporting moderate to severe levels of symptoms. For instance, a substantial 60.4% of respondents note significant changes in mood, while 40.4% experience periods of sadness or depression lasting for days or weeks. Furthermore, continuous feelings of tension or anxiety affect a staggering 42.4% of students severely. These findings underscore the urgent need for targeted interventions and support services to address students' mental health needs effectively. The mean scores and standard deviations provide additional clarity on the severity and variability of these symptoms, emphasizing the importance of proactive measures to promote mental well-being within the student community. The study results indicate that university female students may face various challenges affecting their mental and emotional well-being. These challenges include intense academic pressure, where students must cope with rigorous coursework and frequent exams, potentially increasing levels of stress and anxiety. Additionally, they may encounter social pressures, such as balancing personal relationships with academic performance and managing the social and academic aspects of life. In the context of hormonal changes, female students may be susceptible to mood fluctuations due to changes in their hormones during different phases of the menstrual cycle. In addition to biological and social factors, familial or personal stress may significantly exacerbate mood disorders, with family or personal issues impacting female students and adding further psychological pressure. Life transitions, such as transitioning to university life and adapting to a new environment, could also play a significant role in increasing stress and anxiety levels among female students. Ultimately, genetic and biological factors may also contribute to the onset of mood disorders, as some students may be genetically predisposed to these disorders. Therefore, understanding and providing support for female students through appropriate psychological and healthcare services are vital for promoting their mental health and well-being during their university years.
| Symptoms | Does Not Occur | Mild | Moderate | Severe | Mean | STD | |
|---|---|---|---|---|---|---|---|
| I have noticed significant changes in my mood over the past few weeks. | Frq. | 18 | 113 | 302 | 67 | 2.84 | 0.69 |
| % | 3.6 | 22.6 | 60.4 | 13.4 | |||
| I experience periods of sadness or depression that last for days or weeks. | Frq. | 76 | 156 | 202 | 66 | 2.52 | 0.91 |
| % | 15.2 | 31.2 | 40.4 | 13.2 | |||
| I feel an increase in tension or anxiety continuously. | Frq. | 123 | 86 | 79 | 212 | 2.76 | 1.24 |
| % | 24.6 | 17.2 | 15.8 | 42.4 | |||
| I suffer from a lack of energy or interest in things I used to enjoy. | Frq. | 20 | 86 | 334 | 60 | 2.87 | 0.66 |
| % | 4.0 | 17.2 | 66.8 | 12.0 | |||
| I experience sudden mood swings, such as intense anger or excessive emotions without a clear reason. | Frq. | 44 | 114 | 249 | 93 | 2.78 | 0.85 |
| % | 8.8 | 22.8 | 49.8 | 18.6 | |||
| I have noticed changes in the type and amount of sleep recently. | Frq. | 142 | 94 | 61 | 203 | 2.65 | 1.27 |
| % | 28.4 | 18.8 | 12.2 | 40.6 | |||
| I suffer from changes in appetite, such as loss of appetite or excessive desire to eat. | Frq. | 130 | 94 | 72 | 204 | 2.70 | 1.24 |
| % | 26.0 | 18.8 | 14.4 | 40.8 | |||
| I find it difficult to concentrate on daily tasks or at work. | Frq. | 158 | 94 | 33 | 215 | 2.61 | 1.32 |
| % | 31.6 | 18.8 | 6.6 | 43.0 | |||
| I feel that everyday life problems or family stress significantly affect my mood. | Frq. | 167 | 74 | 92 | 167 | 2.52 | 1.26 |
| % | 33.4 | 14.8 | 18.4 | 33.4 |
The predictive ability of menstrual disorders and hormonal imbalance on the prevalence of mood disorders
To determine the predictive ability of menstrual disorders and hormonal imbalance on the prevalence of mood disorders, a multiple regression analysis was conducted, and the following table illustrates the results of this test (Table 5).
| Sig. | F | Durbin-Watson | R2 | R | Model |
|---|---|---|---|---|---|
| 0.000* | 170.6 | 0.703 | 0.407 | 0.638 | Menstrual disorders and hormonal imbalance - the prevalence of mood disorders |
* Statistically significant at the level of statistical significance (α ≤ 0.05).
The Model Summary table (Table 5) provides a concise overview of the regression model's performance in predicting the prevalence of mood disorders based on menstrual disorders and hormonal imbalance. The statistically significant p-value (Sig. = 0.000) indicates that the overall model is a good fit for the data. The F-value (F = 170.60) suggests that the regression model is significant, implying that at least one of the predictor variables (menstrual disorders or hormonal imbalance) has a significant impact on the prevalence of mood disorders. The Durbin-Watson value (0.703) indicates the absence of autocorrelation in the residuals, suggesting that the assumption of independent errors is not violated. The R-squared value (R2= 0.407) indicates that approximately 40.7% of the variance in the prevalence of mood disorders can be explained by the predictor variables included in the model (Table 6).
| Standardized Coefficients | Unstandardized Coefficients | ||||
|---|---|---|---|---|---|
| Sig. | T | Beta | Std. Error | B | |
| 0.01 | 2.573 | 0.129 | 0.332 | (Constant) | |
| .000* | 14.885 | 0.561 | 0.049 | 0.73 | Menstrual Disorders |
| .000* | 4.049 | 0.153 | 0.035 | 0.142 | Hormonal Imbalance |
The Model Coefficients table (Table 6) presents critical insights into the relationships between predictor variables and the prevalence of mood disorders. The standardized coefficients offer a standardized measure of the impact of each predictor variable, allowing for direct comparison of their influence on the outcome. The unstandardized coefficients, on the other hand, provide valuable information on the magnitude of change in the prevalence of mood disorders for each unit change in the predictor variables. Significant findings emerge from this table, notably the statistically significant coefficients (Sig. < 0.05) associated with both Menstrual Disorders and Hormonal Imbalance. These results suggest that both factors play substantial roles in predicting the prevalence of mood disorders among the studied population. The positive coefficients indicate that an increase in the levels of menstrual disorders and hormonal imbalance is associated with a corresponding increase in the prevalence of mood disorders. Furthermore, the inclusion of the constant term ensures that the model captures any baseline prevalence of mood disorders not explained by the predictor variables. The significant unstandardized coefficients (B) for Menstrual Disorders (0.730) and Hormonal Imbalance (0.142) provide insights into their relative importance in predicting mood disorder prevalence. In conclusion, the Model Coefficients table enriches the study by quantifying the predictive power of Menstrual Disorders and Hormonal Imbalance on mood disorder prevalence. These findings contribute valuable knowledge to the field, emphasizing the importance of addressing menstrual health and hormonal balance in mental health interventions and support strategies. The results indicate that hormonal imbalances and menstrual cycle-related issues can significantly affect women's mental health, particularly in terms of mood disorder onset. Hormonal fluctuations during the menstrual cycle may have a significant impact on emotional balance, leading to feelings of anxiety, tension, and emotional fatigue. Additionally, coping with painful and uncomfortable physical symptoms associated with menstruation, such as abdominal pain and headaches, can lead to high levels of stress and psychological tension. Moreover, these psychological effects may increase the likelihood of mood disorders, such as depression and anxiety. Overall, this complex interaction between biological and psychological factors underscores the importance of comprehensive mental health screening for women experiencing menstrual disorders and hormonal imbalances, along with providing appropriate support and intervention to help them cope with these challenges.
Conclusion
This study serves as a vital cornerstone for understanding the complex interplay between hormonal disorders and mental health among university female students. The results clearly demonstrate that symptoms related to hormonal imbalance and menstrual disorders significantly impact mental health, leading to mood swings, anxiety, and depression in a sizable portion of students. Tables and statistical models highlight that this relationship is not merely associative but directional, as evidenced by the regression analysis indicating that an increase in hormonal disorders and menstrual changes accompanies an increase in the prevalence of mood disorders.
Shedding light on this relationship underscores the urgent need to develop targeted interventions to support the mental health of university students. Interventions focusing on hormonal balance and mental health can alleviate symptoms of menstrual disorders and improve the overall mental and general health of students. Since the results suggest that academic, social, and environmental pressure play significant roles in the experience of university female students, offering multi-level support may be necessary, including mental health services, menstrual health education, and promoting awareness about hormonal balance.
In conclusion, understanding the relationship between menstrual disorders and mental health opens new avenues for research and intervention in the fields of women's health and mental health. By providing comprehensive and targeted support, the well-being of university students can be enhanced, improving their academic and personal experiences.
Administrative implications
The administrative implications of the study findings on menstrual disorders and mental health among university students are multifaceted. They suggest a need for universities to enhance healthcare services, including specialized Care and counseling, to better support students experiencing these issues. Additionally, educational programs and awareness campaigns should be implemented to educate both students and staff about menstrual health and mental well-being. Policy development may be necessary to address issues such as menstrual leave and mental health support services. Resource allocation should prioritize additional healthcare staff, mental health resources, and research programs focusing on women's health. Collaboration with external healthcare providers and advocacy groups can further enhance support for students. Overall, these implications provide guidance for administrators in implementing strategies to promote the health and well-being of university students.
Psychological implications
The psychological implications of the study findings on menstrual disorders and mental health among university students are manifold. Firstly, the research can foster increased awareness and understanding of the psychological impact of menstrual disorders, potentially reducing stigma and shame associated with these conditions. Individuals affected by menstrual disorders may benefit from improved self-perception and coping strategies, as they gain insight into their experiences and feelings. Additionally, the study may prompt universities to enhance mental health services, ensuring students have access to appropriate support. Furthermore, by highlighting the psychological aspects of menstrual health, the research may stimulate further research efforts and educational initiatives aimed at supporting affected individuals and promoting a more empathetic and supportive environment within educational institutions.
Recommendations
Based on the study and the presented results, here are some recommendations that can be adopted:
Develop Education and Awareness Programs: It is recommended to develop educational programs and ongoing awareness campaigns about menstrual health and mental well-being for students and staff at the university. Workshops, seminars, and media can be used to disseminate knowledge and provide emotional support.
Provide Specialized Healthcare Services: It is recommended to provide specialized healthcare services targeting the treatment of menstrual disorders and supporting mental health. These services should include psychological counseling, nutritional guidance, and medication therapy when necessary.
Develop University Policies: The university can develop policies that support students experiencing menstrual disorders and mental health issues. This includes implementing policies for providing sick leave related to menstrual disorders and offering psychological and social support services.
Promote Research and Development: It is recommended to increase funding and support for research focusing on the relationship between menstrual disorders and mental health. Additionally, developing treatment and intervention techniques specifically for students experiencing these conditions is essential.
Provide Psychological and Social Support: Providing psychological and social support programs for students is recommended, whether through individual counseling, support groups, or events that promote mental and social well-being.
References
Alateeq, D., Binsuwaidan, L., Alazwari, L., Algarni, M., Al Hussain, M., Alzahrani, R., & Aljohani, R. (2022). Dysmenorrhea and depressive symptoms among female university students: a descriptive study from Saudi Arabia. The Egyptian journal of neurology, psychiatry and neurosurgery, 58(1), 106. https://doi.org/10.1186/s41983-022-00542-1.
Alblooshi, S., Taylor, M., & Gill, N. (2023). Does menopause elevate the risk for developing depression and anxiety? Results from a systematic review. Australasian psychiatry : bulletin of Royal Australian and New Zealand College of Psychiatrists, 31(2), 165–173. https://doi.org/10.1177/10398562231165439.
Balsom, A. A., & Gordon, J. L. (2021). The relationship between psychological coping and mood across the menstrual cycle among distressed women struggling to conceive. Journal of psychosomatic research, 145, 110465. https://doi.org/10.1016/j.jpsychores.2021.110465.
Chekol, A. T., Reta, Y., Ayinewa, F., Hailu, L., Tesema, M., & Wale, M. A. (2024). Determinants of premenstrual dysphoric disorder and associated factors among regular undergraduate students at Hawassa University Southern, Ethiopia, 2023: institution-based cross-sectional study. BMC public health, 24(1), 1390. https://doi.org/10.1186/s12889-024-18798-y.
Deborah Tolulope Esan, Sharon Ayobami Ariyo, Elizabeth Folabomi Akinlolu, Oluwadamilare Akingbade, Oluwaseyi Isaiah Olabisi, David Bamidele Olawade, Theresa Olaitan Bamigboye, Adesola Adenike Ogunfowokan(2024), Prevalence of dysmenorrhea and its effect on the quality of life of female undergraduate students in Nigeria, Journal of Endometriosis and Uterine Disorders, Volume 5, https://doi.org/10.1016/j.jeud.2024.100059.
Handy, A. B., Greenfield, S. F., Yonkers, K. A., & Payne, L. A. (2022). Psychiatric Symptoms Across the Menstrual Cycle in Adult Women: A Comprehensive Review. Harvard review of psychiatry, 30(2), 100–117. https://doi.org/10.1097/HRP.0000000000000329.
Hromatko, I., & Mikac, U. (2023). A Mid-Cycle Rise in Positive and Drop in Negative Moods among Healthy Young Women: A Pilot Study. Brain sciences, 13(1), 105. https://doi.org/10.3390/brainsci13010105.
https://my.clevelandclinic.org/health/body/22566-hypothalamus.
https://www.britannica.com/science/ovary-animal-and-human.
https://www.healthdirect.gov.au/pituitary-gland.
Hwang, W. J., Lee, T. Y., Kim, N. S., & Kwon, J. S. (2020). The Role of Estrogen Receptors and Their Signaling across Psychiatric Disorders. International journal of molecular sciences, 22(1), 373. https://doi.org/10.3390/ijms22010373.
Itani, R., Soubra, L., Karout, S., Rahme, D., Karout, L., & Khojah, H. M. J. (2022). Primary Dysmenorrhea: Pathophysiology, Diagnosis, and Treatment Updates. Korean journal of family medicine, 43(2), 101–108. https://doi.org/10.4082/kjfm.21.0103.
Özge, A., Domaç, F. M., Tekin, N., Sünbül, E. A., Öksüz, N., Atalar, A. Ç., Çallı, S. Y., Fidan, Y. S., Evlice, A., Beştepe, E. E., İzci, F., Küsbeci, Ö. Y., Demirel, E. A., Velioğlu, S. K., & Ungan, M. (2023). One Patient, Three Providers: A Multidisciplinary Approach to Managing Common Neuropsychiatric Cases. Journal of clinical medicine, 12(17), 5754. https://doi.org/10.3390/jcm12175754.
Rugvedh, P., Gundreddy, P., & Wandile, B. (2023). The Menstrual Cycle's Influence on Sleep Duration and Cardiovascular Health: A Comprehensive Review. Cureus, 15(10), e47292. https://doi.org/10.7759/cureus.47292.
Stephens, M. A., & Wand, G. (2012). Stress and the HPA axis: role of glucocorticoids in alcohol dependence. Alcohol research : current reviews, 34(4), 468–483.
Witchel, S. F., Oberfield, S. E., & Peña, A. S. (2019). Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls. Journal of the Endocrine Society, 3(8), 1545–1573. https://doi.org/10.1210/js.2019-00078.
Zhao, J., Pan, H., Liu, Y., He, Y., Shi, H., & Ge, C. (2023). Interacting Networks of the Hypothalamic-Pituitary-Ovarian Axis Regulate Layer Hens Performance. Genes, 14(1), 141. https://doi.org/10.3390/genes14010141.