Research Article - (2024) Volume 19, Issue 6
Understanding The Connections Between Eating Disorders And Oral Health A Systematic Review
Mohammed Salah Hussein1*, Fatima Ghazi Alshyaokh2, Seham Khalid Zakari3, Razan Mohammed Saleh4, Atheer Salman Alhawiti5, Hussain Mohammed Alheji6, Hassan Mohammed Alhammadi7, Ammar Fawzi Karni8, Faris Talal Alqarihi8, Bader Mohammed H Alqarni9 and Fatimah Ahmed Almarzoug10*Correspondence: Mohammed Salah Hussein, Department of internal medicine, faculty of medicine, Alazhar University hospitals, Cairo, Egypt, Email:
2Dammam Medical Complex - Neurosurgery Department, Saudi Arabia
3harmacist, Jazan University, Saudi Arabia
4Medical intern, Arabian Gulf University, Bahrain
5Medical intern, Tabuk University, Saudi Arabia
6Dentist, Alahssa Health Cluster, Saudi Arabia
7Pediatrics, Maternity and Children Hospital in Dammam, Saudi Arabia
8Physiotherapist, Umm Al-Qura University and Al Wehda FC, Saudi Arabia
9Orthopedic Surgery Department, King Abdulaziz Hospital - Makkah, Saudi Arabia, Saudi Arabia
10General practitioner, Alqatif Health Cluster, Saudi Arabia
Received: 01-Dec-2024 Published: 15-Dec-2024
Abstract
Objectives: To systematically evaluate the available literature regarding the association of eating disorders (EDs) with oral health.
Methods: A search across four databases identified 325 publications. After duplicate removal using Rayyan QCRI and relevance screening, 141 full-text articles were reviewed, leading to the inclusion of 5 studies. Results: We included five studies with a total of 225 diagnosed with EDs and all of them were females. The findings show a clear link between EDs and oral health issues, such as tooth erosion, caries, periodontal disease, and soft tissue damage. Patients with EDs had higher rates of tooth sensitivity, dry mouth, and oral candidiasis. Regular dental visits and educational efforts improved awareness of erosion risks tied to anorexia and bulimia. Although overall erosion rates were similar to controls, ED patients had lower saliva flow and more severe localized erosion. Soft tissue problems like lip redness, cheilitis, and lesions highlight the importance of dental professionals in identifying and managing EDs early.
Conclusion: This review highlights the connection between EDs and oral health problems, stressing the importance of dental professionals in early detection and care. Common issues include tooth erosion, cavities, and soft tissue damage. Although research is limited, evidence suggests dental exams can help identify EDs and enhance patient outcomes. Future studies should focus on larger, standardized approaches to deepen understanding of this link.
Keywords
Eating disorders. Anorexia nervosa. Anorexia bulimia. Oral health. Dental care. Systematic review
Introduction
Unusual eating patterns and upsetting thoughts are hallmarks of EDs, a collection of intricate and possibly fatal behavioral illnesses [1]. Of the eight EDs mentioned in the Diagnostic and Statistical Manual of Mental Disorders 5th Edition's "Feeding and Eating Disorders" chapter, binge eating disorder, anorexia nervosa (AN), and bulimia nervosa (BN) are the ones that are most commonly discussed in the literature [2, 3]. With an estimated lifetime prevalence of 4.60% in males and 8.50% in females, EDs can affect people of various racial backgrounds, ages, and genders [4]. 3.3 million healthy life years are lost each year as a result of the current global increase in EDs, which presents a significant public health burden [5, 6].
The mouth cavity may also experience the bodily effects of EDs. The direct ingestion of acidic foods, such as oranges, energy beverages, or vinegar for reducing appetite, as well as the regurgitation of stomach contents from self-induced vomiting, can cause tooth erosion in people with EDs [7]. Furthermore, self-induced vomiting, hunger, or psychiatric drugs with ant sialagogue properties frequently impair salivary flow in ED patients [8]. Dental caries and periodontal disease, the two most prevalent oral disorders, may become more likely as a result. Nutritional inadequacies, food preferences, or modifications to oral hygiene practices have all been linked to oral mucosal lesions in ED patients [9]. In addition, there have been reports of increased orofacial pain, temporomandibular disorder (TMD), and bruxism habits [10], which may be related to emotional stress, compulsive exercise, or poor general health. Parotid swelling, which frequently results from self-induced vomiting, has been documented in the literature as a presenting feature of BN [11].
EDs are complex psychiatric conditions that seriously affect the general health, often showing the first signs and symptoms in the oral cavity. The symptoms of EDs include vomiting, nutritional deficiencies, and changes in eating behaviors, which can lead to various dental and oral complications such as erosion, caries, and soft tissue lesions. Although it is well known that EDs have serious systemic health consequences, the oral manifestations of the disease are poorly recognized clinically. The relationship between EDs and oral health provides the healthcare professional, especially dentists and orthodontists, with a very important role in early detection and intervention. This systematic review aims to highlight the role of oral health as an indicator of EDs and to indicate the need for an integrated medical-dental approach in the management of the same.
This review was done to systematically evaluate the available literature regarding the association of EDs with oral health in view of describing common oral manifestations, the burden of dental complications, and a possible role of dental professionals in early detection and management of the condition.
Methods
Search strategy
The systematic review was done based on the PRISMA and GATHER criteria. An exhaustive search was made to identify studies related to investigate available evidence on the association of EDs with oral health. The reviewers searched four electronic databases: SCOPUS, Web of Science, Cochrane, and PubMed. After removing any duplicates, we uploaded to Rayyan every abstract and title we could locate using electronic searches. Studies published in the last 10 years (2014-2024) were included. The full texts of the study texts that fulfilled the inclusion criteria according to their abstract or title were retrieved for a detailed analysis. Two independent reviewers assessed the appropriateness of the extracted publications and reviewed inconsistencies.
Study population-selection
The PEO (Population, Exposure, and Outcome) factors were implemented as inclusion criteria for our review: (i) Population: Individuals diagnosed with or suspected of having EDs (e.g., AN, BN, binge eating disorder), (ii) Exposure: Presence of ED-related behaviors, including vomiting, nutritional deficiencies, excessive dieting, or use of medications that impact oral health, (iii) Outcomes: Oral health issues.
Data extraction
Data from studies that satisfied the inclusion requirements were extracted by two objective reviewers using a predetermined and uniform methodology. The following information was retrieved and recorded: (i) First author (ii) Year of publication, (iii) Study design, (iv) Participants’ number, (v) Age, (vi) Gender, (vii) Diagnostic tool of EDs, (viii) Oral health issues, (ix) Main outcomes.
Quality review
We utilized the ROBINS-I technique to evaluate the risk of bias because it allows for extensive assessment of confounding, which is significant because bias owing to omitted variables is common in studies in this field. The ROBINS-I tool is intended to evaluate non-randomized investigations and can be applied to cohort designs in which participants exposed to various staffing levels are monitored over time. Two reviewers separately assessed the risk of bias for each paper, and disagreements were resolved through group discussion [12].
Results
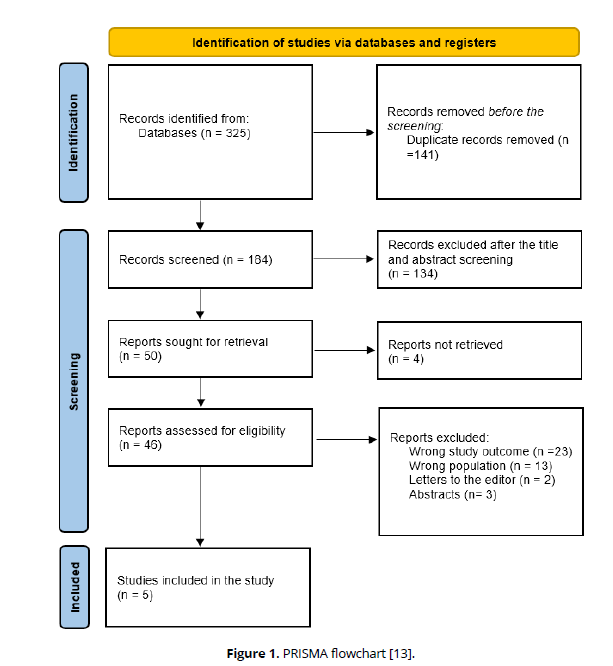
The specified search strategy yielded 325 publications (Figure 1). After removing duplicates (n = 141), 184 trials were evaluated based on title and abstract. Of these, 134 failed to satisfy eligibility criteria, leaving just 46 full-text articles for comprehensive review. A total of 5 satisfied the requirements for eligibility with evidence synthesis for analysis.
Sociodemographic and clinical outcomes
We included five studies with a total of 225 diagnosed with EDs and all of them were females. Regarding the study designs, two were cross-sectional studies [15, 16], two were case-controls [17, 18], and one was a retrospective cohort [14]. Two studies were conducted in the USA [14, 16], one in India [15], one in Portugal [17], and one in Argentina [18].
Other oral health complications among patients with EDs, as were the cases selected for study, included but were not limited to tooth erosion, dental caries, periodontal disease, and soft tissue lesions [14]. The majority of patients with EDs exhibited serious oral signs and symptoms, including but not limited to tooth hypersensitivity, xerostomia, and oral candidiasis. These were significantly higher when compared to the control subjects [15].
It appears that educational interventions and frequent dental visits increased their awareness of possible risks of anorexia nervosa and bulimia nervosa for teeth erosion. Patients who regularly visited dental services were more aware of the implications of oral health for their general health and appearance [16].
In all cases, the mean erosion rate was not statistically different from the control values, even though there was substantial erosion in some subjects; however, the saliva flow rates were always lower among ED patients. Lip erythema, cheilitis, and hemorrhagic lesions were the other soft tissue manifestations. These findings emphasize the important role of dental professionals in diagnosing oral symptoms related to ED and help in its early diagnosis and management [17, 18] (Table 1, Table 2).
| Study ID | Country | Study design | Sociodemographic | Complications | Key findings | |
|---|---|---|---|---|---|---|
| Silverstein et al., 2019 [14] | USA | Retrospective cohort | Participants: 41 Mean age: 25.2 Females |
DSM V | Tooth erosion (76%) Dry mouth (71.1%) Tooth sensitivity (92.7%) Oral candidiasis (34.7%) |
Most patients were aware that AN and BN behaviors could lead to tooth erosion, but only a small portion knew the exact area where it typically occurs. After educational interventions, a much larger group correctly identified the location. Patients who visited the dentist regularly were more likely to believe their oral health positively influenced their appearance, overall health, and happiness. |
| Jugale et al., 2014 [15] | India | Cross-sectional | Participants: 50 Mean age: 21.9 Females |
SCOFF Questionnaire | Tooth erosion (78%) Tooth sensitivity (56%) | The examination revealed a higher prevalence of periomylolysis, dental caries, and tooth sensitivity in suspected cases. The study effectively identified ED, showing significant oral manifestations in those suspected. |
| Dehghan et al., 2023 [16] | USA | Cross-sectional | Participants: 14 Mean age: 33 Females |
DSM V | NS | Compared to the controls, the ED group's stimulated saliva flow rate was noticeably lower, and their DMFT score was greater. The average tooth erosion score of the ED group was not substantially different from the controls, despite the fact that some ED individuals in this pilot research had major tooth erosion. |
| Lourenço et al., 2018 [17] | Portugal | Case-control | Participants: 55 Age range: 28-50 Females |
DSM V | Dental caries, erosion, periodontal disease and lesions in the oral mucosa | Dental caries, erosion, periodontal disease and lesions in the oral mucosa |
| Panico et al., 2018 [18] | Argentina | Case-control | Participants: 65 Age range: 21.6 Females |
DSM V | Soft-tissue lesions and dental erosion | Patients with EDs exhibited lip redness, inflammation of the lips, a yellow-orange hue on the palate, and bleeding lesions. |
| Study ID | Bias due to confounding | Bias in the selection of participants into | Bias in the classification of interventions | Bias due to deviations from the intended interval | Bias due to missing data | Bias in the measurement of outcomes | Bias in the selection of reported result | Overall bias |
|---|---|---|---|---|---|---|---|---|
| Silverstein et al., 2019 [14] | Low | Low | Mod | Low | Low | Low | Mod | Low |
| Jugale et al., 2014 [15] | Mod | Low | Mod | Low | Low | Mod | Low | Moderate |
| Dehghan et al., 2023 [16] | Mod | Mod | Low | Low | Low | Mod | Low | Moderate |
| Lourenço et al., 2018 [17] | Mod | Low | Mod | Low | Low | Mod | Low | Moderate |
| Panico et al., 2018 [18] | Mod | Mod | Low | Low | Low | Mod | Low | Moderate |
Discussion
Discussion: Results from this study also established that EDs had strong significant relations with many complications affecting oral health, emphasizing greater considerations for dental manifestations within cases that raise suspicion for ED and, obviously, when they have been diagnosed. Increased dental erosions, caries, and periodontal involvement seen in patients with EDs represent chronic vomiting associated with the conditions, dietary deficits, and inadequate hygiene habits. Rosten & Newton demonstrated that common oral symptoms in bulimic individuals include dental caries, decreased salivary flow rate, parotid hypertrophy, and tooth erosion. Although the majority of the literature focuses on the impacts of vomiting, this study has demonstrated that antidepressant medication, binge eating, and other dietary practices can also affect a bulimic's oral health [19]. Garbin et al. also reported that patients with bulimia nervosa and anorexia typically have gum and tooth lesions. Therefore, the dental surgeon can lessen the burden of these problems on public health and plays a significant role in their early detection [20].
This review also found that the diagnosis of soft tissue lesions, lip erythema, and oral candidiasis further emphasizes the systemic nature of EDs and their effects on oral tissues. Regular dental checkups and selective education seem to increase awareness and maybe decrease some of the oral health risks in ED patients. However, differences in the severity of erosion and flow rates of saliva indicate the need for an individual approach in assessment and treatment. A similar review also stated the significance of including bulimia signs and symptoms in the dental curriculum since dental professionals are frequently the first to recognize bulimia symptoms. Dentists are well-positioned to counsel bulimic patients on maintaining good dental hygiene after vomiting and to minimize their use of acidic foods and beverages [19].
Frequent tooth brushing [21] may aggravate the greater prevalence of dental erosion in ED patients, which may be caused by excessive consumption of acidic beverages or stomach acid [22]. Given its function in flushing, neutralizing acid, and demineralizing the dental enamel with its supersaturated amount of calcium and phosphate ions, decreased salivary flow may also lessen the degree of protection that teeth receive from erosion [23].
The increased frequency of oral lesions may be explained by nutritional deficits brought on by selective feeding patterns as well as physical and chemical stress from self-induced purging. People with orange-yellow palates who participated in Panico's study said they took supplements of carotene. The greater frequency of repetitive tongue, lip, or cheek biting and hemorrhagic lesions observed in this group may be caused by self-harming behaviors and emotional disturbances linked to EDs [18].
Dentists may be in a good position to provide early identification and intervention for EDs according to the characteristic oral manifestations. Regular dental consultations may provide opportunities for identifying warning signs-tooth erosion, xerostomia, and soft tissue lesions-which may indicate the need for referral for psychological or medical evaluation. Educational programs in the oral signs of EDs among dental practitioners increase their capabilities for early detection. This could also allow for improved overall patient outcomes and diminish the long-term effects of EDs on oral health.
Strengths and Limitations
The systematic review approach has ensured completeness in analyzing the existing literature and has given a comprehensive overview regarding the relation between EDs and oral health. The diversity in the study designs, populations, and geographical locations increases the generalizability of the findings. Duplicate removal and screening were made more accurate and efficient by using Rayyan QCRI. However, only a limited number of studies that met the inclusion criteria allow broad conclusions to be drawn. Variability in study designs, sample sizes, and diagnostic criteria introduces heterogeneity that may affect the consistency of results. Some of the studies did not provide detailed information on certain oral health outcomes, which reduced the depth of analysis.
Conclusion
The review highlighted the strong association of EDs with oral health complications and the role of dental professionals in early detection and management. The high prevalence of tooth erosion, dental caries, and soft tissue lesions among ED patients justifies an integrated approach to care. Although the limited nature of the available literature restricts some generalizations, the results confirm that dental assessments are an important diagnostic tool in EDs and contribute to overall patient care. Further studies are required with larger samples and more consistent methodologies to help establish a clearer relationship between EDs and oral health.
References
Hambleton A, Pepin G, Le A, Maloney D, Touyz S, Maguire S. Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature. J Eat Disord. 2022;10(1):132.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. 2013. Available from: https://www.psychiatry.org/psychiatrists/practice/dsm
Silén Y, Keski-Rahkonen A. Worldwide prevalence of DSM-5 eating disorders among young people. Curr Opin Psychiatry. 2022;35(6):362–71.
Streatfeild J, Hickson J, Austin SB, Hutcheson R, Kandel JS, Lampert JG, et al. Social and economic cost of eating disorders in the United States: evidence to inform policy action. Int J Eat Disord. 2021;54(5):851–68.
Galmiche M, Dechelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–13.
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521–7.
Hermont AP, Oliveira PA, Martins CC, Paiva SM, Pordeus IA, Auad SM. Tooth erosion and eating disorders: a systematic review and meta-analysis. PLoS One. 2014;9(11):e111123.
Cockburn N, Pradhan A, Taing MW, Kisely S, Ford PJ. Oral health impacts of medications used to treat mental illness. J Affect Disord. 2017; 223:184–93.
Lo Russo L, Campisi G, Di Fede O, Di Liberto C, Panzarella V, Lo Muzio L. Oral manifestations of eating disorders: a critical review. Oral Dis. 2008;14(6):479–84.
Emodi-Perlman A, Yoffe T, Rosenberg N, Eli I, Alter Z, Winocur E. Prevalence of psychologic, dental, and temporomandibular signs and symptoms among chronic eating disorder patients: a comparative control study. J Orofac Pain. 2008;22(3):201–8.
Buchanan JA, Fortune F. Bilateral parotid enlargement as a presenting feature of bulimia nervosa in a post-adolescent male. Postgrad Med J. 1994;70(819):27–30.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. bmj. 2016 Oct 12;355.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Prisma-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015 Dec; 4:1-9.
Silverstein LS, Haggerty C, Sams L, Phillips C, Roberts MW. Impact of an oral health education intervention among a group of patients with eating disorders (anorexia nervosa and bulimia nervosa). Journal of eating disorders. 2019 Dec; 7:1-6.
Jugale PV, Pramila M, Murthy AK, Rangath S. Oral manifestations of suspected eating disorders among women of 20-25 years in Bangalore City, India. Journal of health, population, and nutrition. 2014 Mar;32(1):46.
Dehghan M, Tantbirojn D, Harrison J, Stewart CW, Johnson N, Tolley EA, Zhang YH. Oral Health and Behavior Patterns of Women with Eating Disorders—A Clinical Pilot Study. Life. 2023 Dec 3;13(12):2297.
Lourenço M, Azevedo Á, Brandão I, Gomes PS. Orofacial manifestations in outpatients with anorexia nervosa and bulimia nervosa focusing on the vomiting behavior. Clinical oral investigations. 2018 Jun; 22:1915-22.
Panico R, Piemonte E, Lazos J, Gilligan G, Zampini A, Lanfranchi H. Oral mucosal lesions in anorexia nervosa, bulimia nervosa and EDNOS. Journal of psychiatric research. 2018 Jan 1; 96:178-82.
Rosten A, Newton T. The impact of bulimia nervosa on oral health: A review of the literature. British dental journal. 2017 Oct 13;223(7):533-9.
Garbin CA, Martins RJ, de Melo Belila N, Garbin AJ. Oral manifestations in patients with anorexia and bulimia nervosa: a systematic review. Journal of Public Health. 2020 Dec; 28:765-71.
Johansson AK, Norring C, Unell L, Johansson A. Eating disorders and oral health: a matched case–control study. European journal of oral sciences. 2012 Feb;120(1):61-8.
Chiba FY, Sumida DH, Moimaz SA, Chaves Neto AH, Nakamune AC, Garbin AJ, Garbin CA. Periodontal condition, changes in salivary biochemical parameters, and oral health‐related quality of life in patients with anorexia and bulimia nervosa. Journal of periodontology. 2019 Dec;90(12):1423-30.
Dehghan M, Tantbirojn D, Harrison J, Stewart CW, Johnson N, Tolley EA, Zhang YH. Oral Health and Behavior Patterns of Women with Eating Disorders—A Clinical Pilot Study. Life. 2023 Dec 3;13(12):2297.