Research Article - (2024) Volume 19, Issue 5
Updates In Diagnosis And Management Of Postmenopausal Bleeding And Its Associated Anxiety A Systematic Review
Ahmed Baker A Alshaikh1*, Fawaz E Edris2, Aryam Abdullah Alhassan3, Raghad Faris Ismail Alsabilah4, Farah Turki Alfuhigi3 and Shafi Ali Alsharari5*Correspondence: Ahmed Baker A Alshaikh, Associated Professor and Consultant obstetrics and gynecology. College of medicine. Jouf University, KSA, Email:
2Professor and Consultant of Obstetrics and Gynecology, College of Medicine, Umm AlQura University, Makkah, Saudi Arabia
3Medical Student, College of medicine. Jouf University, KSA
4General Practitioner, Resident Obgyn, Domat AljandalGeneral Hospital, Saudi Arabia
5General Practitioner, Resident of Emergency Department, AlQurayyat General Hospital, Saudi Arabia
Received: 12-Oct-2024 Published: 22-Oct-2024
Abstract
Objectives: To review the diagnosis and management of postmenopausal bleeding (PMB).
Methods: We conducted a thorough search of PubMed, SCOPUS, Web of Science, and Google Scholar to find pertinent literature. Rayyan QRCI was utilized during the entire process.
Results: We included twelve studies with a total of 1859 participants. Hysteroscopy is the most acceptable tool to initially manage cases with PMB to stop the bleeding. Endometrial biopsies have been demonstrated to be beneficial in cases when malignancy is suspected. Spiral artery power and velocity addition Doppler flow mapping can help distinguish between benign disease and endometrial cancer in patients with thicker endometrium. TVS with endometrial thickness (ET) assessment is a non-invasive, easily accessible, and costeffective method of diagnosis, it should be the first line of study in the examination of women with PMB who have suspected endometrial disease. SIS is a well-tolerated, safe, and uncomplicated treatment that yields excellent diagnostic accuracy. Diagnosis of the cause of bleeding and its management will relieve the associated anxiety.
Conclusion: In clinical practice, PMB is an important factor for healthcare professionals. There is an ongoing debate on the best investigative order for patients with PMB. The goal of future studies should be to obtain higher accuracy with less interference. Blind biopsies should be avoided as they have the potential to overlook endometrial disease, particularly when it is localized. To detect intrauterine pathology, hysteroscopy with biopsy under visualization is a more accurate operation and needs to be preferred over blind methods. A common gynecologic problem that is never to be disregarded is PMB.
Keywords
Postmenopausal bleeding; Diagnosis; Management; Systematic review.
Introduction
The permanent cessation of menstruation following a year of amenorrhea is known as natural menopause. It is a diagnosis made in retrospect. In western nations, the menopause typically occurs at the age of 51.4 [1]. The "perimenopause," which is the period that precedes menopause by four years, is marked by irregular periods, a change in hormone levels, such as elevated follicle stimulating hormone, and clinical symptoms like hot flashes, insomnia, and dry vagina [2, 3].
The synthesis of progesterone, estrogens, and, to a lesser extent, androgens—particularly testosterone, dehydroepiandrosterone sulfate, androstenedione—decreases significantly regardless of the cause(s) of menopause. While vaginal atrophy, osteoporosis, and changes in the metabolic profile that increase the risk of heart attacks are among the long-term repercussions, hot flushes and other vasomotor symptoms play a significant role in the menopausal transition [4]. The reproductive organs atrophy gradually as a result of decreased amounts of progesterone and estrogens [5]. The endometrium experiences progressive atrophy during menopause as well; in the absence of cyclic hormonal stimulation, this atrophy takes place. Exogenous hormone therapy used often during menopause may alter the endometrium, which may multiply in response to hormonal stimulation and result in PMB [6].
A typical gynecologic complaint is PMB [7, 8]. After menopause, the prevalence of PMB declines with time, from about 400/1000 women/year immediately following menopause to 42/1000 women/year three years later [7].
A thorough medical history should be obtained at the patient's initial evaluation, with a focus on PMB risk factors. It is crucial to first establish the menopausal state of patients, particularly those who are younger, by getting information on their most recent menstrual cycle and making sure that a full year has passed since the last amenorrhea. An epidemiological investigation showed that whereas the risk of endometrial cancer rises with the years of menopause, the incidence of PMB falls with age [7].
Other organ symptoms, such as those related to the urinary tract that could indicate urological causes of bleeding or that point to gastrointestinal disorders like bloody stools or painful defecation, should also be investigated. A complete medical history, including family history, should be collected. It is necessary to record risk factors for endometrial cancer, such as obesity, diabetes, hypertension, and some genetic diseases like Lynch syndrome, which causes non-polyposis colorectal cancer. It is important to ask about medications that may contribute to PMB, such as nutritional supplements, hormone therapy, tamoxifen, and anticoagulants [7]. This systematic review investigates the recently published literature on the diagnosis and management of PMB.
Methodology
Study Design and Duration
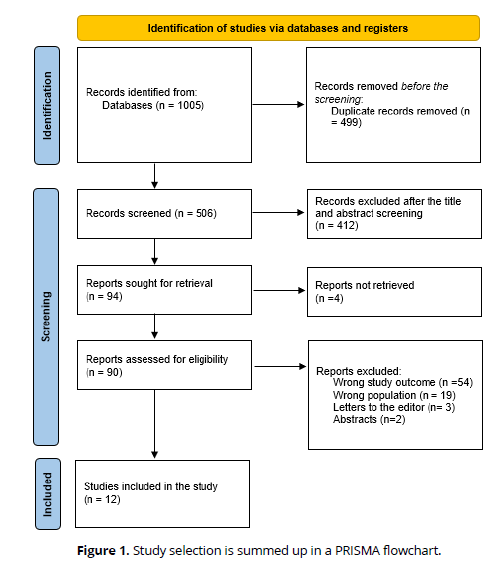
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) standards were followed in this systematic review [9]. In April 2024, the systematic review got started.
Search strategy
To find relevant material, a comprehensive search was conducted using four key databases: PubMed, SCOPUS, Web of Science, and Google Scholar. We searched through databases that contained only English content, paying attention to the unique requirements of each. To find the relevant papers, we converted the following keywords to PubMed Mesh terms; "Postmenopausal bleeding," "Abnormal uterine bleeding," "Diagnosis," and "Management." "OR," "AND," and "NOT," three boolean operators, matched the necessary keywords. Full-text English publications, freely accessible articles, and human trials were among the search results.
Selection criteria
We considered the following criteria for inclusion in this review:
- Any study design that discussed the diagnosis and management of PMB.
- Studies conducted within the last five years (2019-2024).
- Only human subjects.
- English language.
- Free accessible articles.
Data extraction
Two output verifications of the search method were conducted using Rayyan (QCRI) [10]. By using inclusion/exclusion criteria, the researchers evaluated how relevant the abstracts and titles were to the combined search results. The reviewers carefully considered every manuscript that met the inclusion requirements. The authors talked about ways to resolve conflicts. A pre-made data extraction form was used to upload the approved study. The authors extracted data on the study title, authors, study year, country, participants, age, parity, state of hormonal therapy, diagnostic tools, management, and the main outcomes.
Strategy for data synthesis
Summary tables using information from relevant studies were compiled to provide a qualitative assessment of the research's findings and components. The best technique for using the data from the included study articles was chosen after the data for the systematic review was gathered.
Results
Search results
The systematic search produced 1005 study articles in total, of which 499 duplicates were eliminated. After 506 studies had their titles and abstracts screened, 412 were not included. After 94 reports were requested to be retrieved, 4 articles were not found. After screening 90 studies for full-text assessment, 54 were rejected due to incorrect study results, 19 were rejected due to incorrect population type, 3 articles were editor's letters, and 2 were abstracts. This systematic review included twelve eligible study articles. A synopsis of the procedure for choosing studies is provided in (Figure 1).
Characteristics of the included studies
Table (1) shows the sociodemographic details of the research articles that are included. Our results included twelve studies with a total of 1859 participants. Eight studies were prospective in nature [11, 13, 16, 18-22] and only two were retrospective in nature [12, 15]. Five studies were conducted in india [13, 18, 19, 20, 22], two in Egypt [16, 21], two in Vietnam [11, 14], one in the USA [12], one in Saudi Arabia [15], and one in the UK [17].
Clinical characteristics
Management
Table (2) reveals the clinical characteristics including the diagnosis and management of women with PMB. As PMB is a pathological condition that represents a symptom of other major pathology that could be benign or malignant, there are few studies that discuss the management of our condition. One study stated that hysteroscopy is the most acceptable tool to initially manage cases with PMB to stop the bleeding. Experienced surgeons can safely and effectively perform hysteroscopic endometrial resection in conjunction with resection of intrauterine pathology in women with PMB [15].
Diagnosis
Hysteroscopy and biopsy
Endometrial biopsies have been demonstrated to be beneficial in cases when malignancy is suspected [12]. Hysteroscopic viewing is essential and has been linked to greater sensitivity in diagnosing intrauterine disease in women with symptomatic uterine hemorrhage [12, 15, 16, 19, 22]. Another study repoted that hysteroscopy should only be used in instances with poorly defined endometrial lining, recurrent or chronic bleeding, and endometrial thickness greater than 5 mm, regardless of endometrial echotexture, in low-resource settings [18]. Saad et al. reported that hysteroscopy's diagnostic accuracy in identifying submucosal myoma was superior to that of SIS and TVS [21].
Doppler
Spiral artery power and velocity addition Doppler flow mapping can help distinguish between benign disease and endometrial cancer in patients with thicker endometrium [13, 14].
Non-invasive methods (US, TVS, SIS)
Ultrasound has good inter-rater reliability when used to diagnose benign endometrial polyps, endometrial cancer, and uniformly thickened endometrium in women with PMB [11, 17]. Other studies reported that because TVS with endometrial thickness (ET) assessment is a non-invasive, easily accessible, and cost-effective method of diagnosis, it should be the first line of study in the examination of women with PMB who have suspected endometrial disease [18, 22]. Another found that SIS is a well-tolerated, safe, and uncomplicated treatment that yields excellent diagnostic accuracy [20] (Table 1, Table 2).
| Study | Study design | City | Participants | Age range |
|---|---|---|---|---|
| Nguyen & Nguyen, 2023 [11] | Prospective interventional | Vietnam | 150 | >40 |
| Ferrando et al., 2023 [12] | Retrospective cohort | USA | 689 | 49 |
| Nasheeha et al., 2021 [13] | Prospective observational | India | 50 | 41-60 |
| Nguyen et al., 2022 [14] | Cross-sectional | Vietnam | 60 | 45-80 |
| Vilos et al., 2020 [15] | Retrospective cohort | Saudi Arabia | 151 | 50-87 |
| Abdel Hameed et al., 2022 [16] | Prospective cohort | Egypt | 237 | 48-80 |
| Wong et al., 2021 [17] | Cross-sectional | UK | 52 | 57-69 |
| Vasudeva et al., 2022 [18] | Prospective cohort | India | 82 | 50-65 |
| Nisha & Sunitha, 2019 [19] | Prospective cohort | India | 100 | 51.5 |
| Bharti & Dewan, 2020 [20] | Prospective cross-sectional | India | 138 | 56.7 |
| Saad et al., 2020 [21] | Prospective interventional | Egypt | 50 | 45-63 |
| Devabhaktuni et al., 2020 [22] | Prospective cohort | India | 100 | 45-79 |
| Study | Parity (range) | Hormonal therapy (%) | Diagnostic tool | Management | Main outcomes |
|---|---|---|---|---|---|
| Nguyen & Nguyen, 2023 [11] | NM | NM | Sonography and CBC | NM | While assessing intrauterine anomalies in women experiencing perimenopausal and PMB, hemoglobin concentration and fundamental sonographic characteristics should be taken into consideration. In uterine intracavitary diseases, the prognosis of anemia can be ascertained using ultrasonic indices of uterine size. |
| Ferrando et al., 2023 [12] | 0-10 | 69 (10%) | Hysteroscopy and endometrial biopsy | NM | Endometrial biopsies have been demonstrated to be beneficial in cases when malignancy is suspected; nevertheless, blind evaluation of the endometrial cavity for a conclusive diagnosis should be abandoned when benign localized pathology is detected. Hysteroscopic viewing has been linked to greater sensitivity in diagnosing intrauterine disease in women with symptomatic uterine hemorrhage. |
| Nasheeha et al., 2021 [13] | NM | NM | Uterine and spiral artery Doppler | NM | Spiral artery power and velocity addition Doppler flow mapping can help distinguish between benign disease and endometrial cancer in patients with thicker endometrium. |
| Nguyen et al., 2022 [14] | NM | NM | ET and uterine artery Doppler parameters | NM | The Doppler indices of uterine artery endometrial thickness, resistance index, pulsatility index, and peak systolic velocity may be useful in distinguishing between benign and malignant endometrial alterations. There appears to be a correlation between the higher stages of endometrial cancer and pulsed ultrasonic Doppler velocimetry. |
| Vilos et al., 2020 [15] | 0-7 | 83 (54.9%) | Hysteroscopy | Hysteroscopy | For the majority of intrauterine pathology, including nonatypical endometrial hyperplasia and some cases of atypical hyperplasia and endometrial cancer, as well as for the diagnosis of all cases, experienced surgeons can safely and effectively perform hysteroscopic endometrial resection in conjunction with resection of intrauterine pathology in women with PMB. |
| AbdelHameed et al., 2022 [16] | NM | NM | Hysteroscopy | NM | The essential instrument for accurately identifying a range of endouterine disorders in women with PMB is hysteroscopy. |
| Wong et al., 2021 [17] | NM | NM | US | NM | The findings demonstrate that subjective pattern recognition has good inter-rater reliability when used to diagnose benign endometrial polyps, EC, and uniformly thickened endometrium in women with PMB by ultrasound. |
| Vasudeva et al., 2022 [18] | 89% are multipara | NM | TVS and Hysteroscopy | NM | Because TVS with ET assessment is a non-invasive, easily accessible, and cost-effective method of diagnosis, it should be the first line of study in the examination of women with PMB who have suspected endometrial disease. Despite being more sensitive and specific, hysteroscopy should only be used in instances with poorly defined endometrial lining, recurrent or chronic bleeding, and endometrial thickness greater than 5 mm, regardless of endometrial echotexture, in low-resource settings. |
| Nisha & Sunitha, 2019 [19] | NM | NM | TVS and Hysteroscopy | NM | For the assessment of post-menopausal bleeding, hysteroscopy, and transvaginal ultrasonography are both options. When comparing transvaginal ultrasonography and histology, hysteroscopy has a stronger correlation. When a woman experiences bleeding after menopause, hysteroscopy is the most effective method for identifying endometrial abnormalities. |
| Bharti & Dewan, 2020 [20] | NM | NM | SIS, TVU, and hysteroscopy | NM | SIS is a well-tolerated, safe, and uncomplicated treatment that yields excellent diagnostic accuracy. For endometrial examination, SIS appears to be similar to hysteroscopy. |
| Saad et al., 2020 [21] | 0-7 | NM | SIS and hysteroscopy | NM | Regarding pathological diagnosis, hysteroscopy's diagnostic accuracy in identifying submucosal myoma was superior to that of SIS and TVS. When it came to the diagnosis of polypoid lesions in the uterine cavity, SIS and hysteroscopy agreed 100% of the time, making them more accurate than TVS. When it came to pathological diagnosis, SIS's diagnostic accuracy was superior to both hysteroscopy and TVS in the detection of endometrial hyperplasia. |
| Devabhaktuni et al., 2020 [22] | NM | NM | Hysteroscopy | NM | ET measurement TVS, US, and ideally endometrial echo complex is required for women experiencing PMB. |
*NM=Not-mentioned
Discussion
For the menopausal woman with vaginal tract pathology to receive an effective course of treatment, precise diagnostic procedures are necessary. One typical gynecologic ailment is PMB. As up to 10% of bleeding cases are caused by cancer or premalignant diseases, the doctor needs to look into the source of the bleeding. In the past, dilatation and curettage (D&C) performed under general anesthesia was the gold-standard diagnostic technique for PMB, but novel, less invasive, office-based methods of examination have arisen [23].
As PMB is a pathological condition that represents a symptom of other major pathology that could be benign or malignant, few studies discuss the management of our condition in this review. One study stated that hysteroscopy is the most acceptable tool to initially manage cases with PMB to stop the bleeding. Experienced surgeons can safely and effectively perform hysteroscopic endometrial resection in conjunction with resection of intrauterine pathology in women with PMB [15].
We also found that endometrial biopsies have been demonstrated to be beneficial in cases when malignancy is suspected [12]. Hysteroscopic viewing is essential and has been linked to greater sensitivity in diagnosing intrauterine disease in women with PMB [12, 15, 16, 19, 22]; however, another study reported that hysteroscopy should only be used in instances with poorly defined endometrial lining, recurrent or chronic bleeding, and endometrial thickness greater than 5 mm, regardless of endometrial echotexture, in low-resource settings [18]. Wortman, reported that when compared to hysteroscopy with target eye biopsy, diagnostic hysteroscopy is the gold standard technique because it can subjectively assess the size and characteristics of the lesion with a reported sensitivity of 58–99%, specificity of 87–100%, positive predictive value (PPV) of 21–100%, and NPV of 66–99% [24]. Despite the excellent accuracy of visual hysteroscopy, a guided biopsy is always necessary to rule out the existence of malignant diseases. Compared to alternative blind sampling techniques like D&C) and pipelle, which may fail to sample a sizable amount of the endometrial cavity, office hysteroscopy-guided biopsies have higher accuracy. Consequently, while examining endometrial polyps, blind biopsy should not be performed as a diagnostic technique, per the guidelines [25].
We also found that Ultrasound has good inter-rater reliability when used to diagnose benign endometrial polyps, endometrial cancer, and uniformly thickened endometrium in women with PMB [11, 17]. A systematic review and meta-analysis by Vroom et al. demonstrated that women with PMB can be categorized for additional therapy with hysteroscopy or expectant management using saline contrast sonohysterography. All women who are managing their pregnancy should be advised to visit their gynecologist again for additional diagnostic testing if they experience recurrent bleeding [26].
Other studies in this review reported that because TVS with ET assessment is a non-invasive, easily accessible, and cost-effective method of diagnosis, it should be the first line of study in the examination of women with PMB who have suspected endometrial disease [18, 22]. For a preliminary assessment of a patient with PMB, transvaginal ultrasonography is thought to be appropriate [27]. Often seen as the "endometrial lining," the endometrial echo complex (ECC) is a double layer with homogeneous sonolucency. It ought to be measured with the uterus seen in a sagittal perspective at its thickest point. Regarding the threshold value for a normal ECC in a postmenopausal woman, there is no agreement. According to multiple investigations, patients with PMB who have a homogenous ECC of less than 4 mm have a larger than 99% negative predictive value for endometrial cancer [27-29]. To firmly rule out endometrial cancer in patients with PMB, various endometrial thickness cutoff values have been suggested as a non-invasive method.
Another study in this review found that SIS is a well-tolerated, safe, and uncomplicated treatment that yields excellent diagnostic accuracy [20]. In order to improve the assessment of intracavitary lesions, SIS entails the intrauterine injection of normal saline solution. According to a recent systematic review and meta-analysis, SIS has a sensitivity of 86.5% (95% CI 63.6–100%) and a specificity of 91.1% (95% CI 63.2–100%) when it comes to diagnosing endometrial disease in patients with PMB [30]. Ultimately, the authors estimated a sensitivity of 95% and a specificity of 88% utilizing pooled data from systematic reviews conducted to assess the diagnostic accuracy of SIS in the examination of women with irregular uterine bleeding. However, postmenopausal women's (87%) total SIS success rate for endometrial disease diagnosis was substantially lower than that of premenopausal women (p < 0.01) [31].
Conclusion
In clinical practice, PMB is an important factor for healthcare professionals. There is an ongoing debate on the best investigative order for patients with PMB. The goal of future studies should be to obtain higher accuracy with less interference. Blind biopsies should be avoided as they have the potential to overlook endometrial disease, particularly when it is localized. In order to detect intrauterine pathology, hysteroscopy with biopsy under visualization is a more accurate operation and need to be preferred over blind methods. A common gynecologic problem that is never to be disregarded is PMB.
References
Sydora BC, Yuksel N, Veltri NL, et al. Patient characteristics, menopause symptoms, and care provided at an interdisciplinary menopause clinic: retrospective chart review. Menopause 2018; 25:102-5.
Burger HG. Unpredictable endocrinology of the menopause transition: clinical, diagnostic and management implications. Menopause Int 2011; 17:153-4.
Harlow SD, Gass M, Hall JE, et al. Executive summary of the stages of reproductive aging workshop þ 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab 2012; 97:1159-68.
Grady D. Clinical practice. Management of menopausal symptoms. N Engl J Med 2006; 355:2338–47.
Gupta A, Desai A, Bhatt S. Imaging of the endometrium: physiologic changes and diseases: women’s imaging. Radiographics 2017; 37:2206-7.
Winter TC, 3rd. Endometrial thickness in symptomatic postmenopausal patients receiving hormone replacement therapy or tamoxifen. Radiographics 2018; 38:658–9.
Astrup K, Olivarius N de F. Frequency of spontaneously occurring postmenopausal bleeding in the general population. Acta Obstet Gynecol Scand 2004; 83:203-7.
Raouf SA, Gupta P, Papaioannou S, Pradhan P. Endometrial thickness for invasive investigations in women with postmenopausal bleeding. Climacteric 2011; 14:117-20.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., ... & Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International journal of surgery, 88, 105906.
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyana web and mobile app for systematic reviews. Systematic reviews, 5, 1-10.
Nguyen PN, Nguyen VT. Assessment of paraclinical characteristics in peri-and postmenopausal bleeding women: ¿is there a correlation between hemoglobin levels and ultrasonic indices?. Journal of Taibah University Medical Sciences. 2023 Jun 1;18(3):488-98.
Ferrando CA, Lintel MK, Bradley LD. Comparing endometrial biopsy results with hysteroscopic pathology in women presenting with abnormal and postmenopausal uterine bleeding. Journal of Gynecology Obstetrics and Human Reproduction. 2023 Dec 1;52(10):102685.
Nasheeha N, Poomalar GK. Diagnostic accuracy of uterine artery and spiral artery Doppler for evaluation of endometrial pathology in postmenopausal bleeding. Journal of Gynecology Obstetrics and Human Reproduction. 2021 Dec 1;50(10):102209.
Nguyen PN. Endometrial thickness and uterine artery Doppler parameters as soft markers for prediction of endometrial cancer in postmenopausal bleeding women: a cross-sectional study at tertiary referral hospitals from Vietnam. Obstetrics & Gynecology Science. 2022 Sep;65(5):430.
Vilos GA, AlJasser R, Vilos AG, Oraif A, Abduljabar H, Abu-Rafea B. Histopathology and clinical outcomes of 151 women with postmenopausal bleeding treated with resectoscopic surgery. Journal of Minimally Invasive Gynecology. 2020 Mar 1;27(3):763-73.
AbdelHameed AM, Rabei NH, Dikary MM, Farid LA. Hysteroscopy in the Evaluation of Postmenopausal Bleeding. The Egyptian Journal of Hospital Medicine. 2022 Oct 1;89(2):6297-304.
Wong M, Thanatsis N, Amin T, Bean E, Madhvani K, Jurkovic D. Ultrasound diagnosis of endometrial cancer by subjective pattern recognition in women with postmenopausal bleeding: prospective inter‐rater agreement and reliability study. Ultrasound in Obstetrics & Gynecology. 2021 Mar;57(3):471-7.
Vasudeva S, Baxi DA, Mishra A. A prospective study on postmenopausal bleeding-causes and its diagnosis using transvaginal ultrasound and hysteroscopy. International Journal of Reproduction, Contraception, Obstetrics and Gynecology.;11(9):2.
Nisha E, Sunitha HB. Comparison of evaluation of postmenopausal bleeding between transvaginal sonography, hysteroscopy and histopathology.
Bharti S, Dewan R. Evaluation of endometrial pathology in women with postmenopausal bleeding by saline infusion sonography and hysteroscopy. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2020 May 1;9(5):2068-73.
Saad SA, Murad AW, Moustafa ST, Fawzy HE. Saline Infusion Sonography Versus Hysteroscopy in Postmenopausal Bleeding. Benha Journal of Applied Sciences. 2020 Dec 1;5(8 part (1) -(2):293-300.
Devabhaktuni P, Allani P, Komatlapalli S, Ksheerasagara RR. Hysteroscopy in one hundred cases of postmenopausal uterine bleeding, in the detection of uterine cancer and atypical endometrial hyperplasia. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2020 Jun 1;9(6):2253-62.
Carugno J. Clinical management of vaginal bleeding in postmenopausal women. Climacteric. 2020 Jul 3;23(4):343-9.
Wortman M. “See-and-treat” hysteroscopy in the management of endometrial polyps. Surg Technol Int 2016; 28:177–84.
American Association of Gynecologic. AAGL practice report: practice guidelines for the diagnosis and management of endometrial polyps. J Minim Invasive Gynecol 2012; 19:3-10.
Vroom AJ, Timmermans A, Bongers MY, Van den Heuvel ER, Geomini PM, Van Hanegem N. Diagnostic accuracy of saline contrast sonohysterography in detecting endometrial polyps in women with postmenopausal bleeding: systematic review and meta‐analysis. Ultrasound in Obstetrics & Gynecology. 2019 Jul;54(1):28-34.
ACOG Committee Opinion No. 734: The role of transvaginal ultrasonography in evaluating the endometrium of women with postmenopausal bleeding. Obstet Gynecol 2018;131: e124-e9.
Timmermans A, Opmeer BC, Khan KS, et al. Endometrial thickness measurement for detecting endometrial cancer in women with postmenopausal bleeding: a systematic review and meta-analysis. Obstet Gynecol 2010; 116:160–7.
Smith-Bindman R, Weiss E, Feldstein V. How thick is too thick? When endometrial thickness should prompt biopsy in postmenopausal women without vaginal bleeding. Ultrasound Obstet Gynecol 2004; 24:558–65.
Kamel HS, Darwish AM, Mohamed SA. Comparison of transvaginal ultrasonography and vaginal sonohysterography in the detection of endometrial polyps. Acta Obstet Gynecol Scand 2000; 79:60-4.
Kroon CD, Bock GH, Dieben SWM, Jansen FW. Saline contrast hysterosonography in abnormal uterine bleeding: a systematic review and meta-analysis. BJOG 2003; 110:938-47.